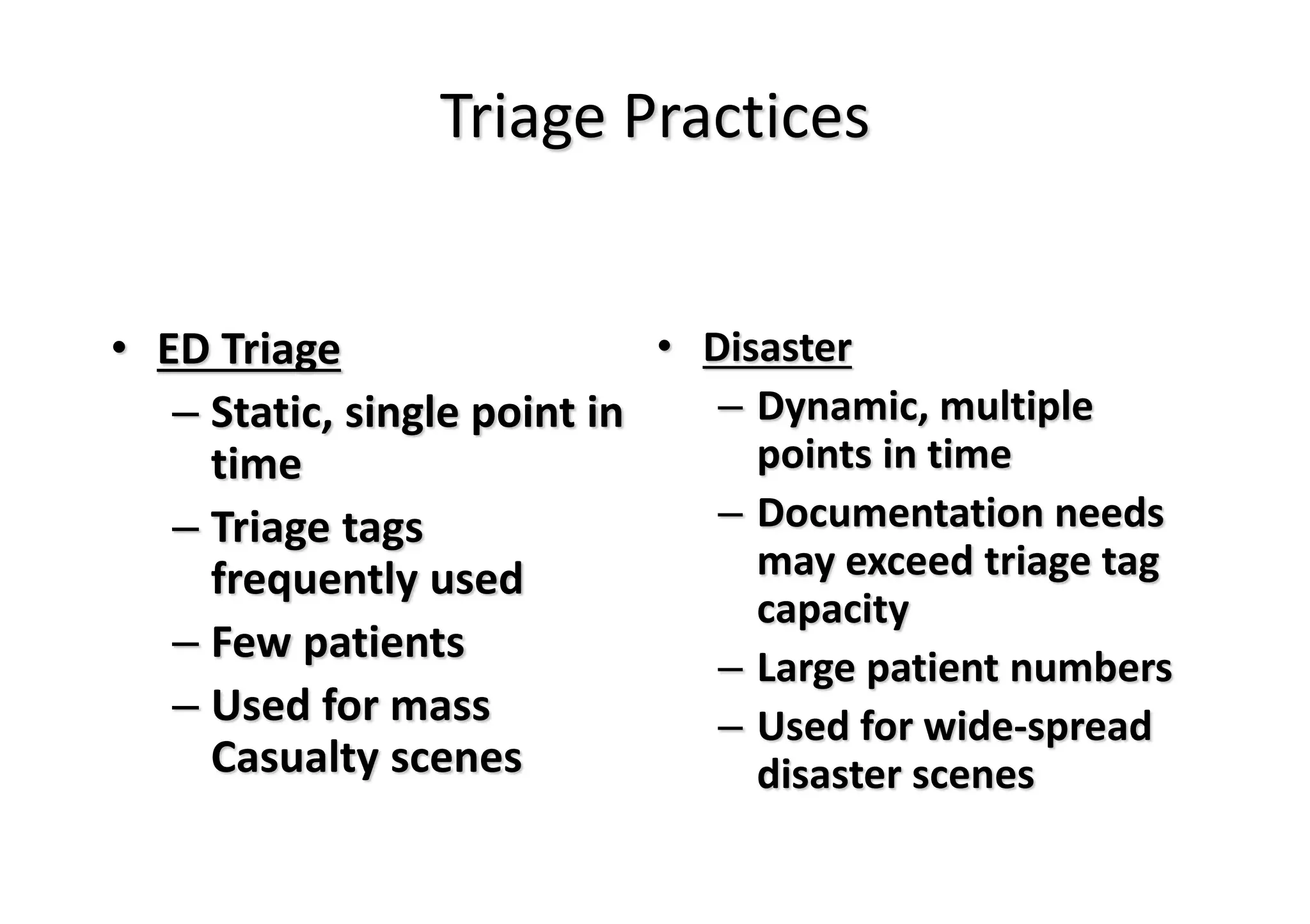
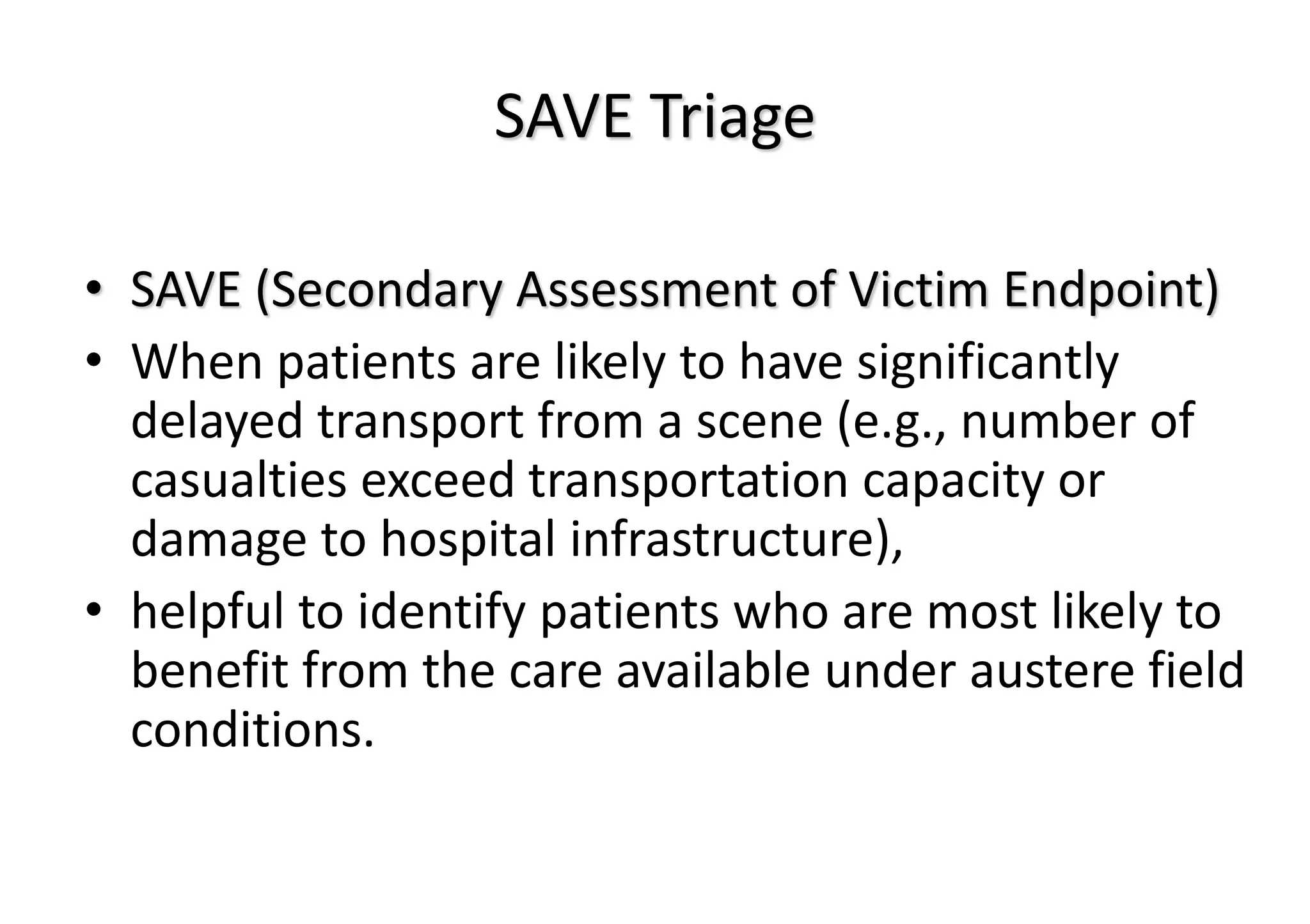
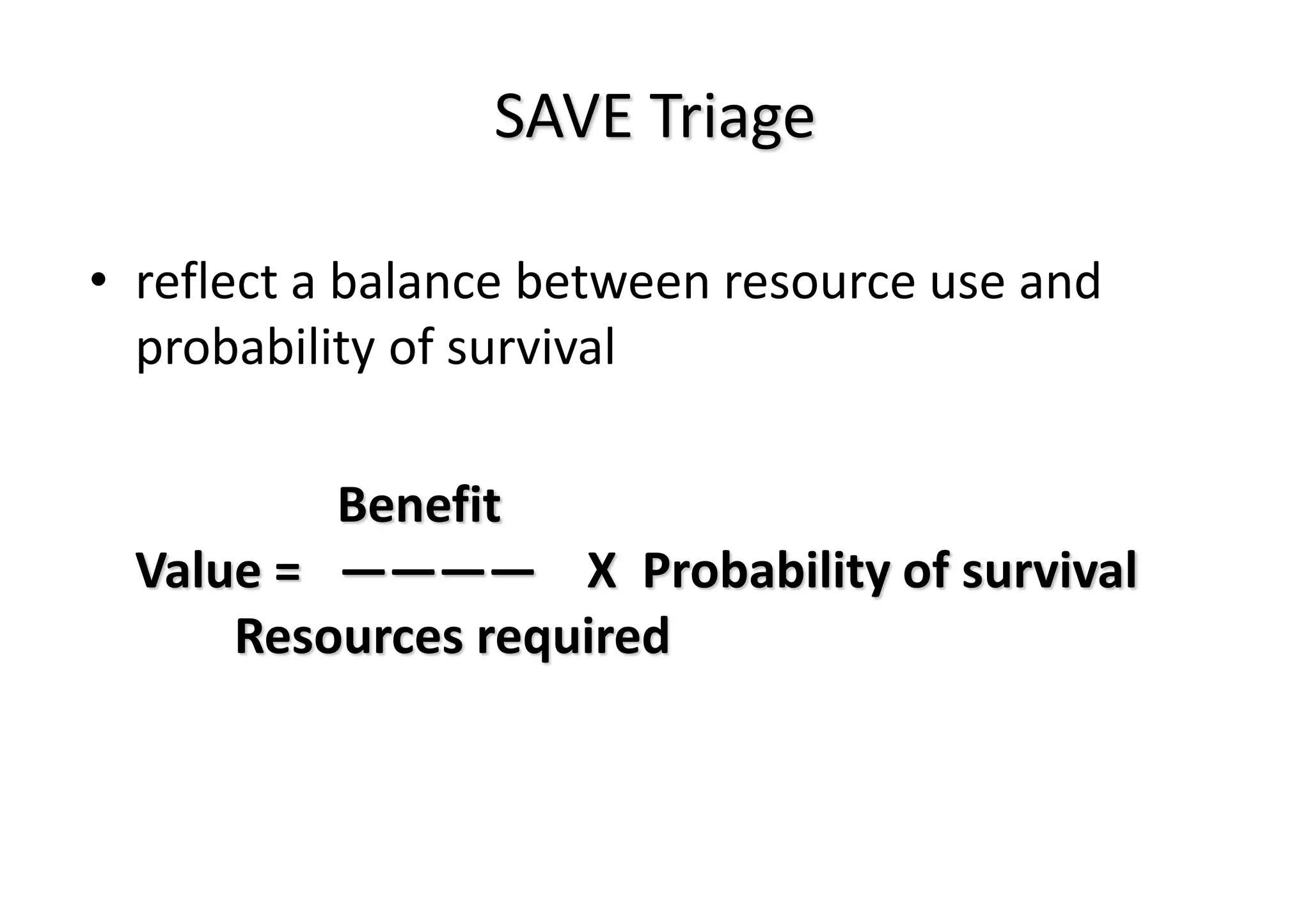
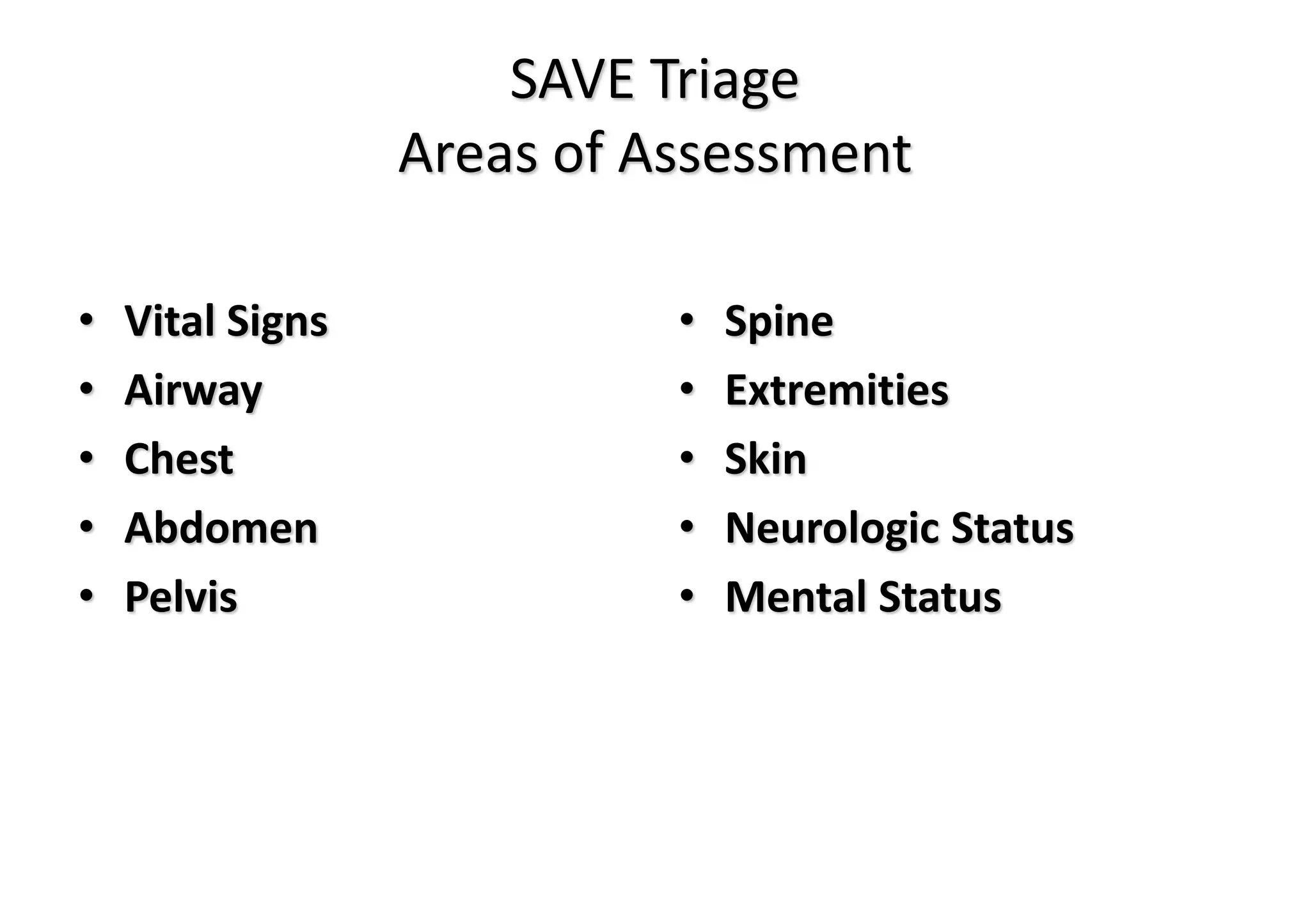
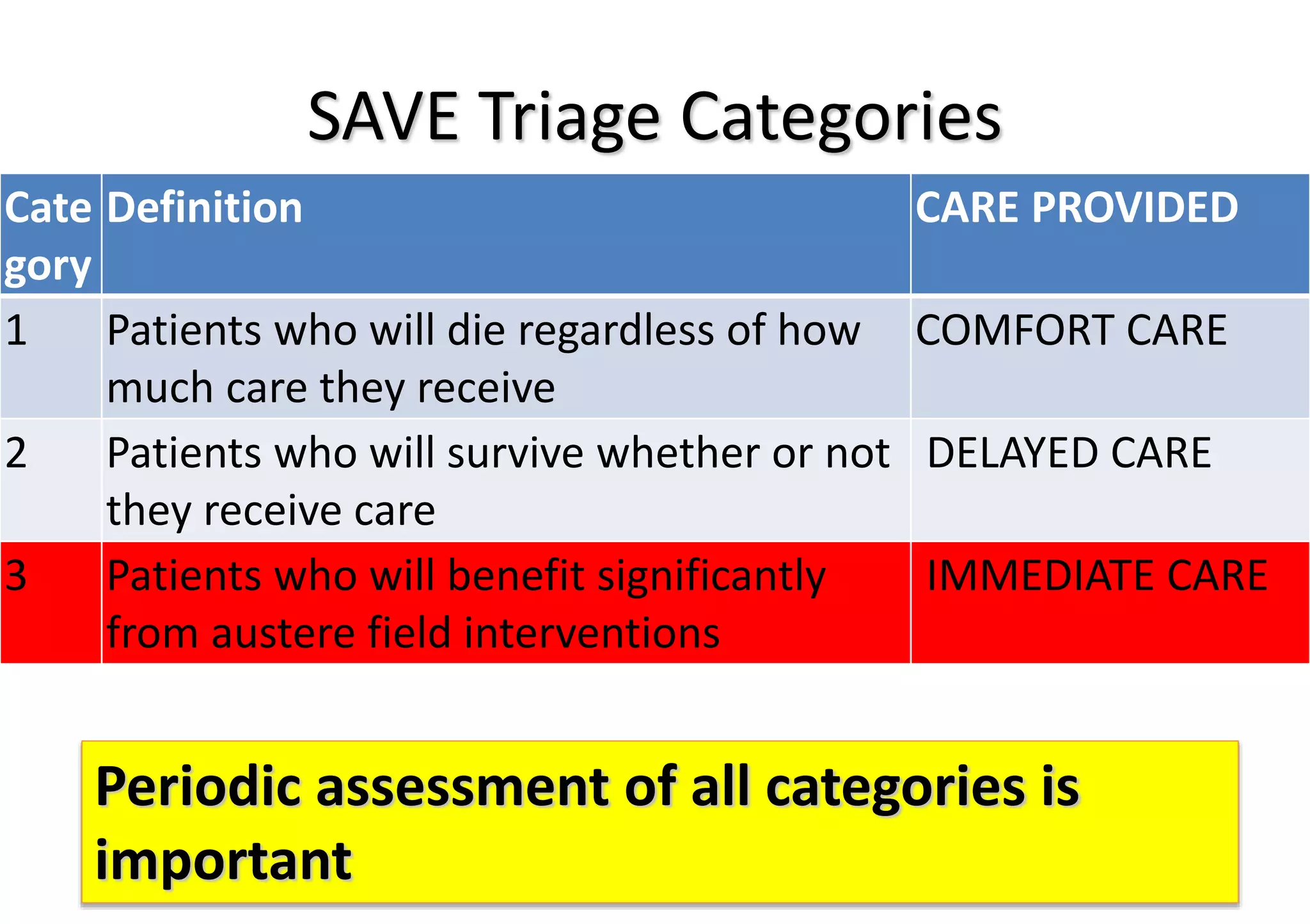
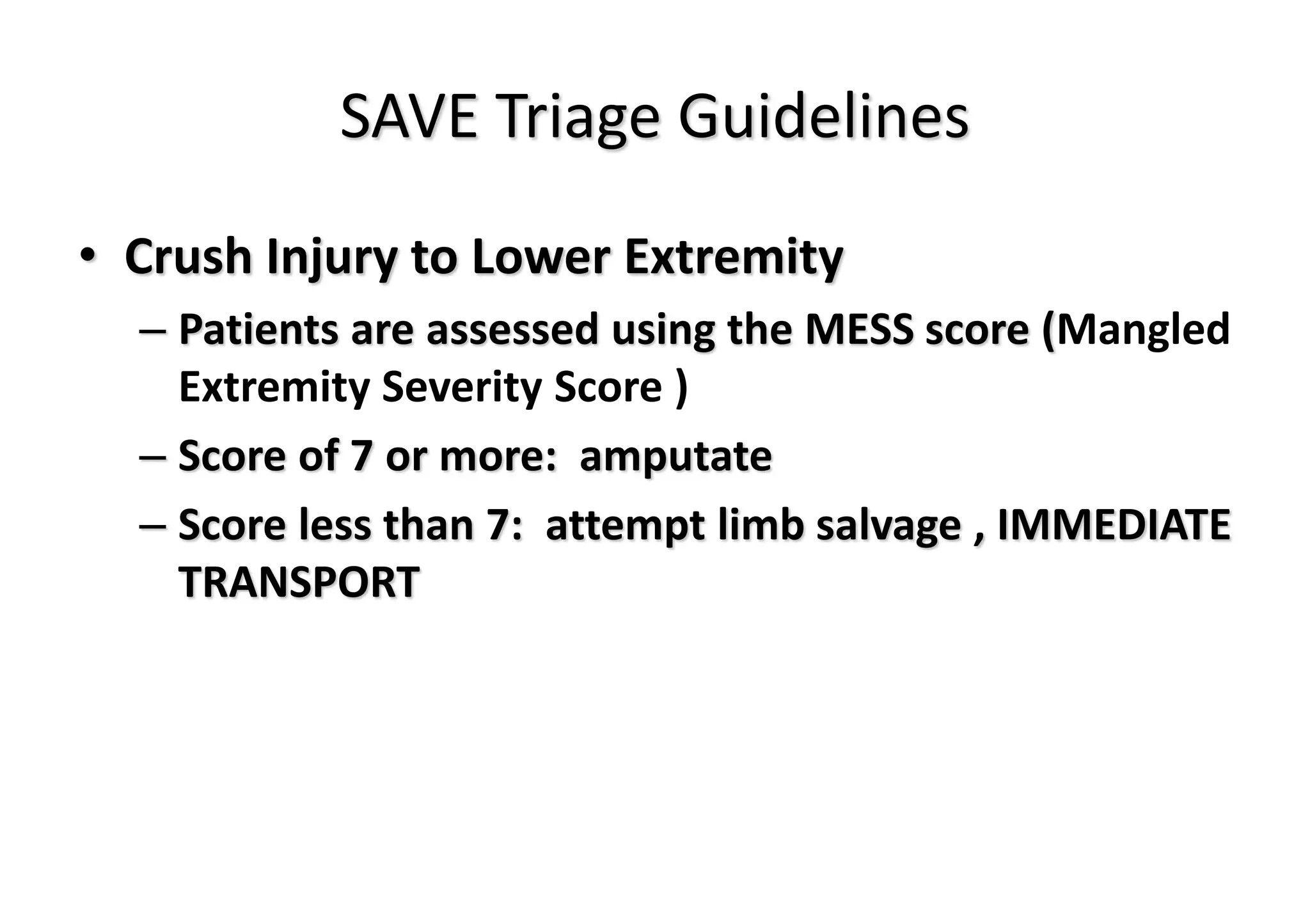
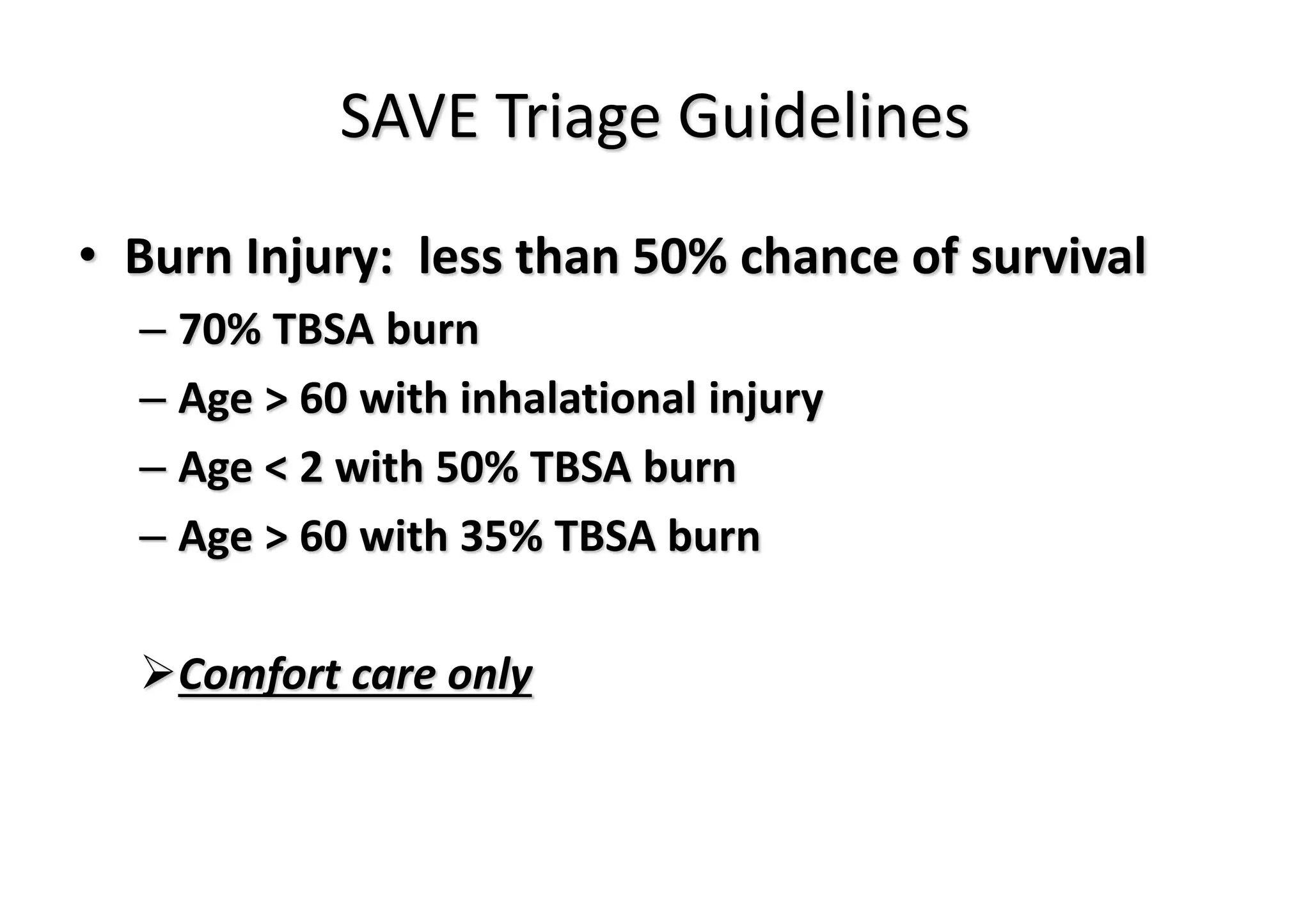
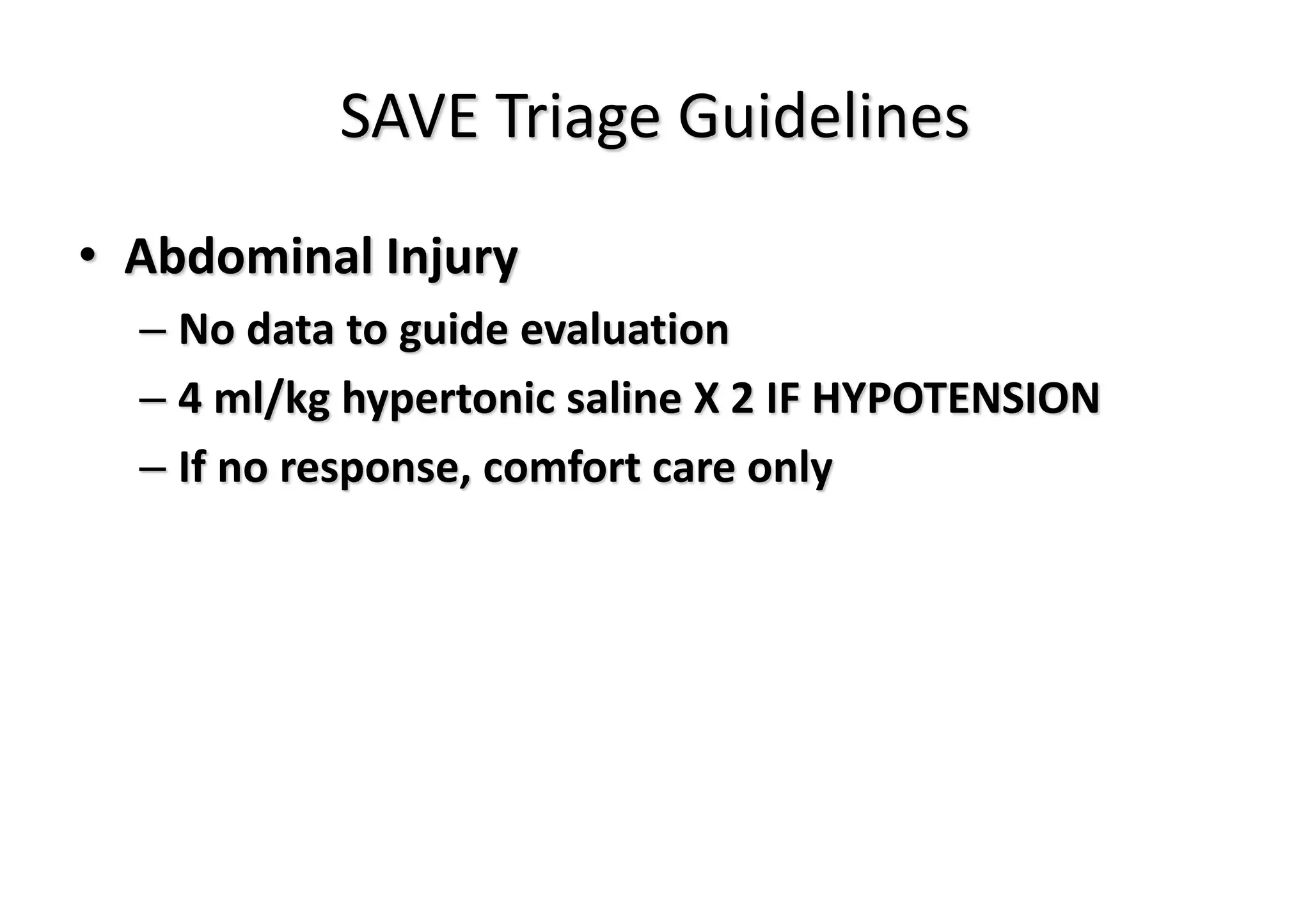
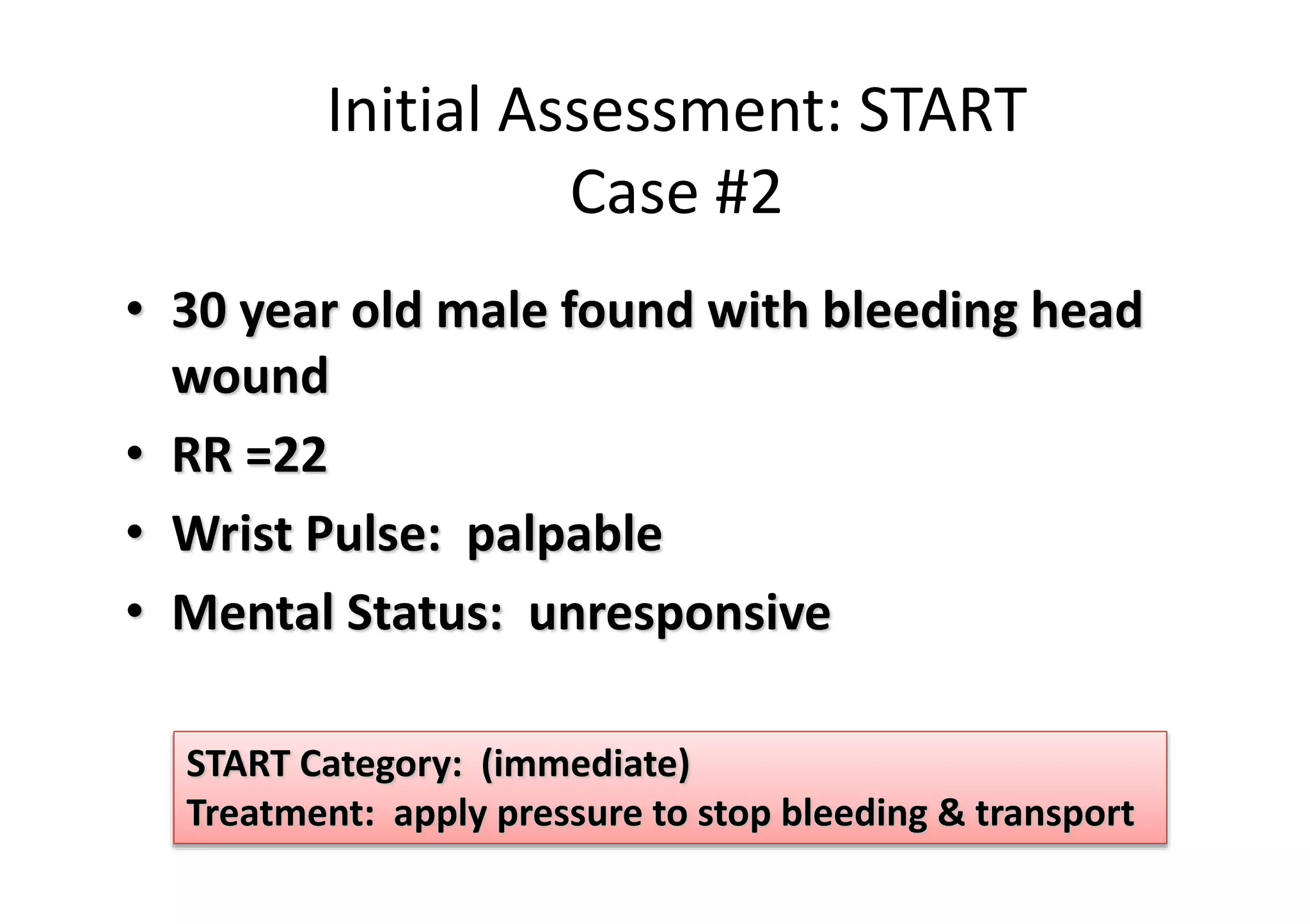
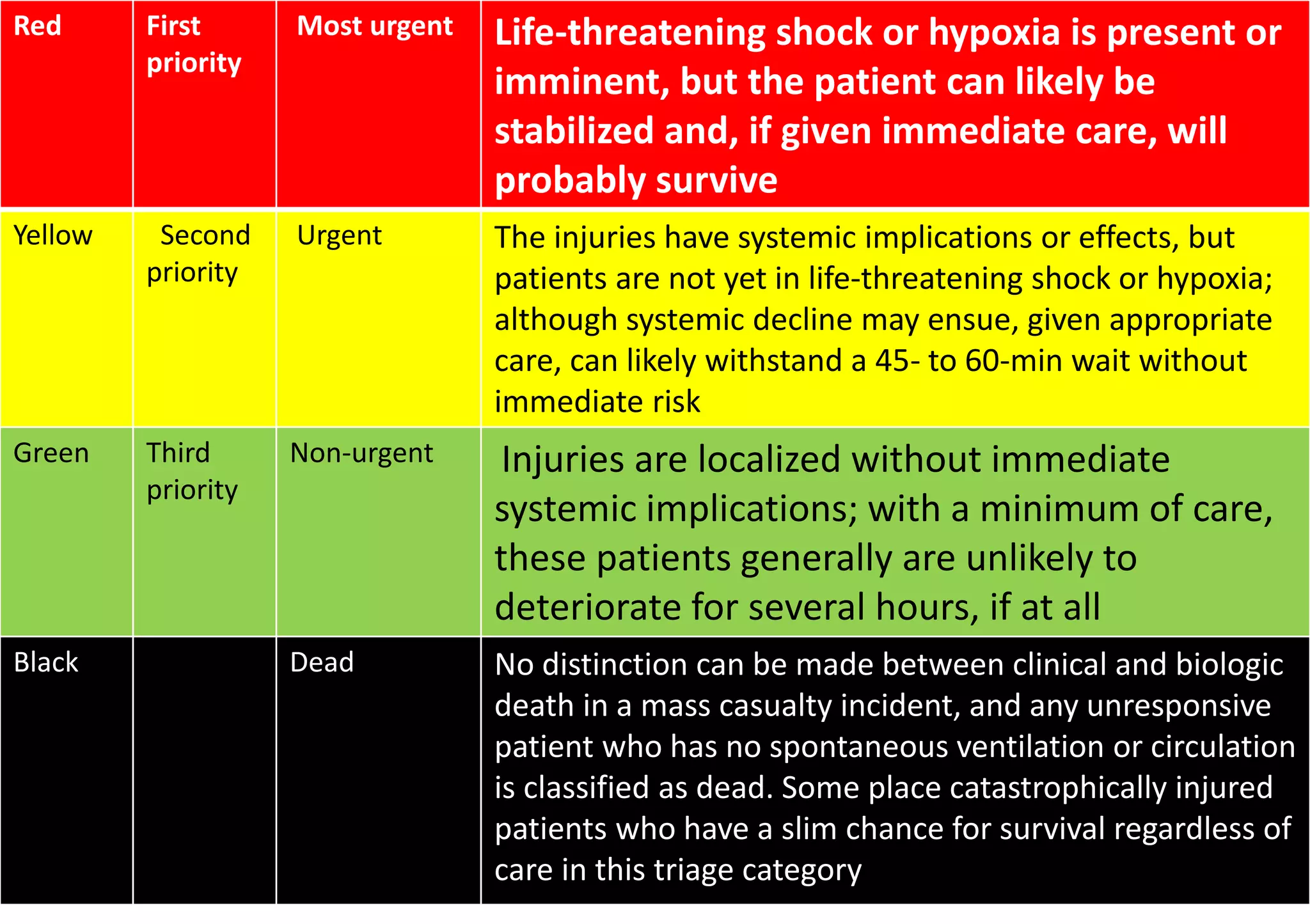
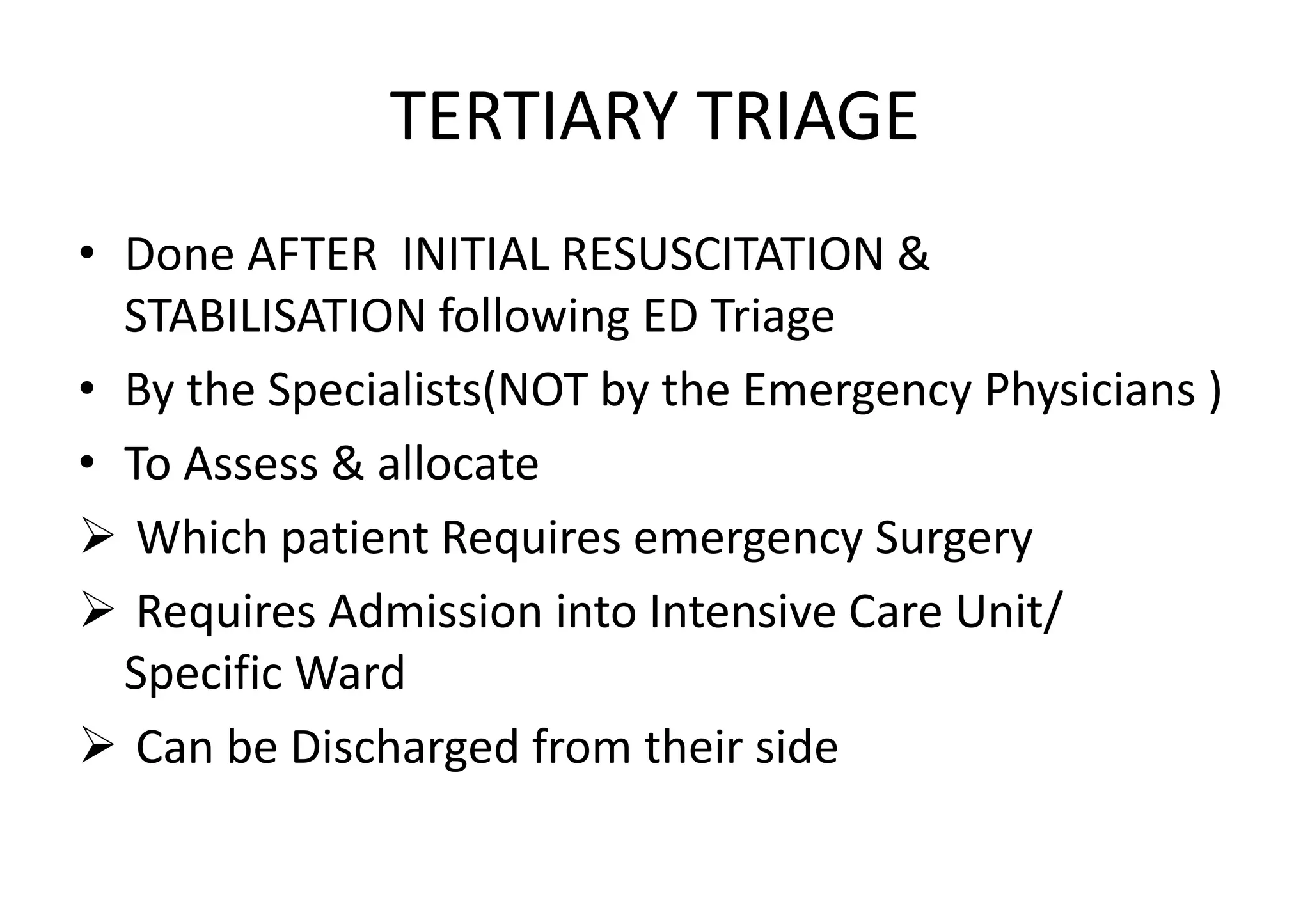
Triage is the process of prioritizing patients according to the urgency of their need for care. It aims to ensure patients are treated in order of clinical urgency and receive timely care. There are three main types of triage - primary triage in the field, secondary triage in the emergency department, and tertiary triage by specialists. The START and SAVE methods are used for disaster triage in the field to categorize patients into immediate, delayed, or minimal care/expectant groups. In the ED, patients are assigned colors based on their condition - red for most urgent, yellow intermediate, green less urgent, and black for deceased. Documentation, equipment, and designated triage teams are needed to properly conduct triage