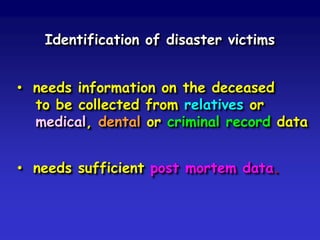
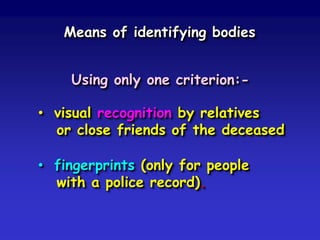
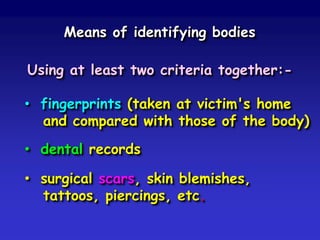
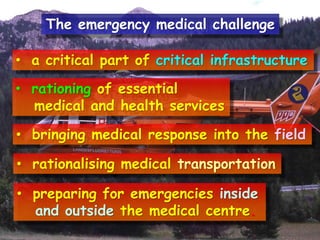
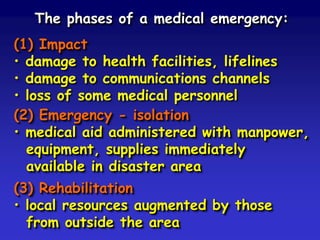
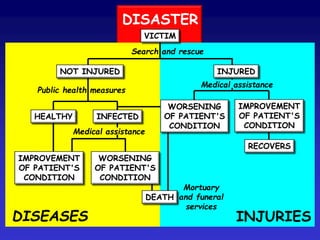
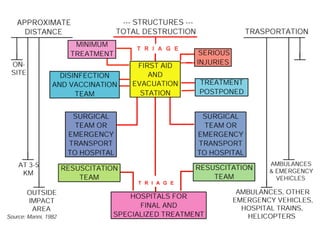
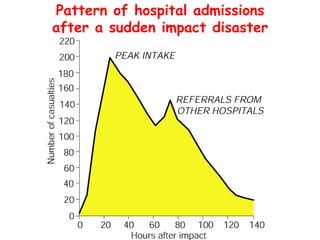
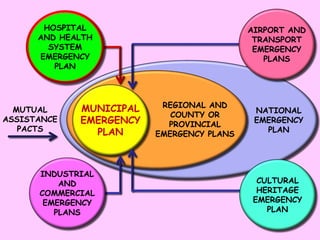
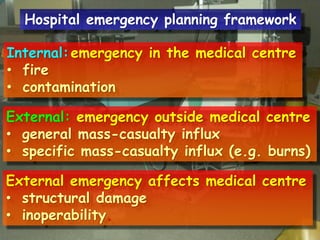
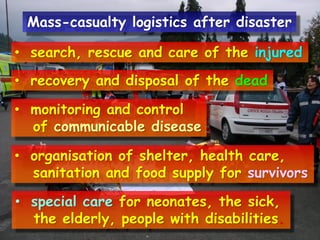
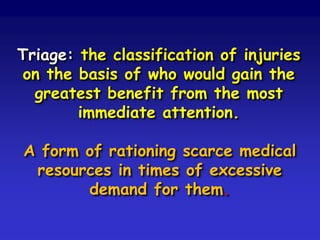
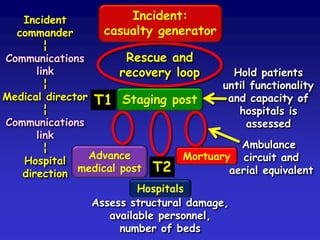
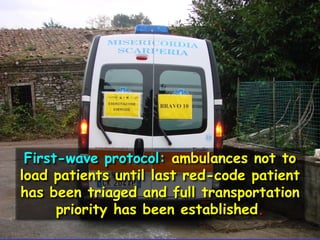
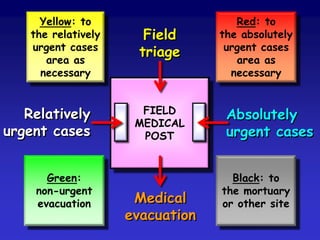
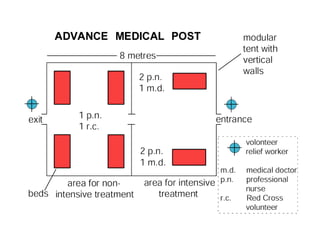
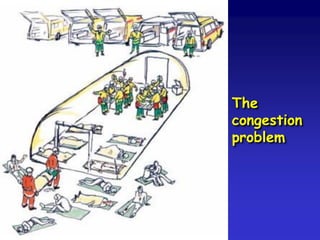
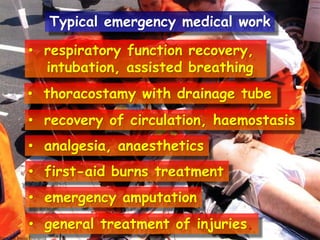
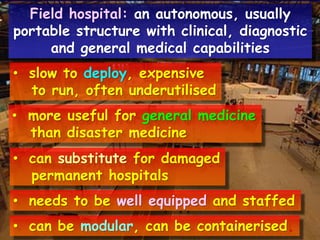
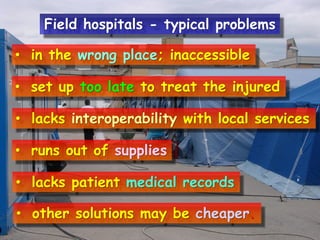
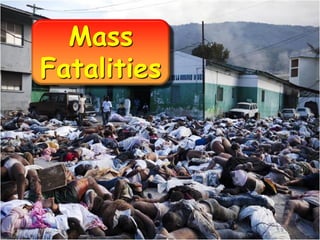
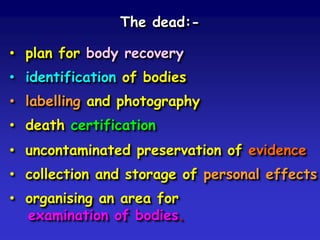
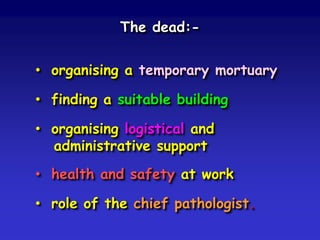
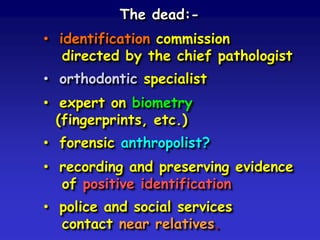
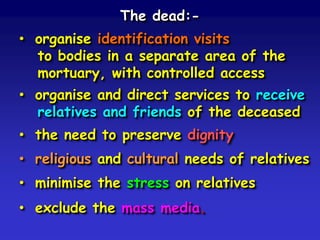
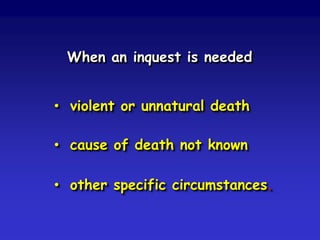
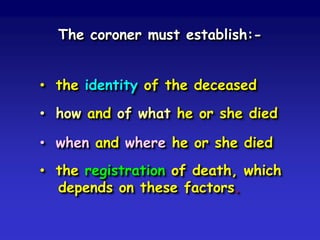
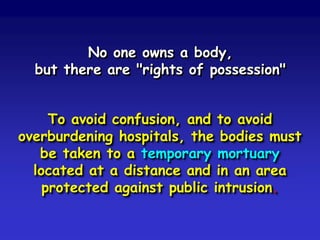
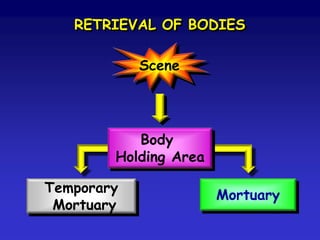
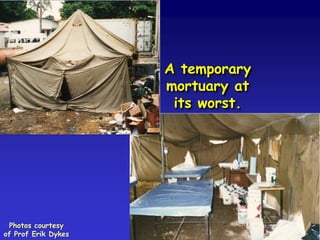
This document discusses emergency medical service planning for disasters. It covers triage, which involves classifying patients based on who would benefit most from immediate medical attention. An advance medical post provides initial stabilization near the disaster site. Field hospitals can substitute for damaged hospitals but have challenges. Mass casualty management involves search and rescue, medical care, disease monitoring, and mortuary services. Temporary morgues are needed to identify victims and determine causes of death. Overall, effective EMS planning requires coordination across various emergency response plans and medical facilities.


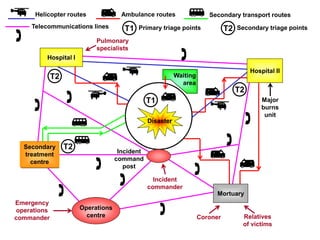
![Plan for the following medical aid:• rescue: medical assistance during SAR
• first aid: advance medical post
• hospital: main or prolonged treatment
• transfer: inter-hospital movement
[HEMS / road ambulance interaction].](https://image.slidesharecdn.com/medicalemergencyplanning-131101113618-phpapp02/85/Medical-emergency-planning-20-320.jpg)









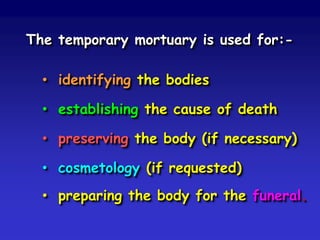

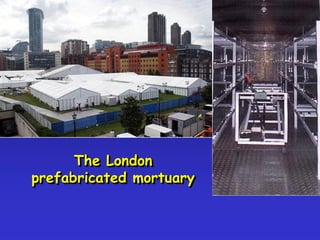

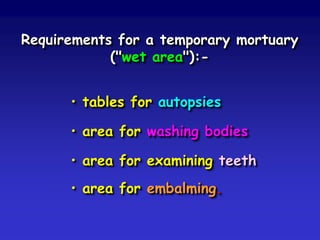
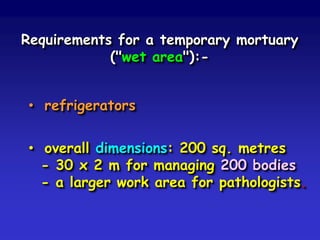
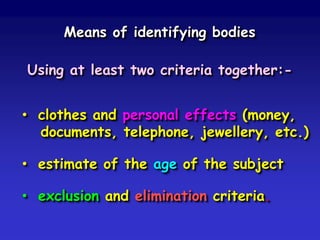
![Requirements for a temporary mortuary
("dry area"):• a room for body identification
• an office for the coroner
• an x-ray room [+ developing facilities]
• showers and toilets
• area for stockpiling coffins
• screens for the mortuary entrance.](https://image.slidesharecdn.com/medicalemergencyplanning-131101113618-phpapp02/85/Medical-emergency-planning-66-320.jpg)