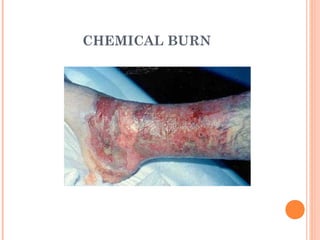
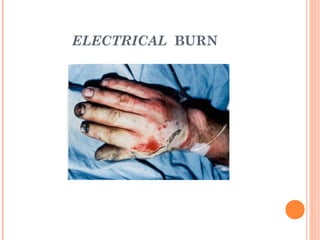
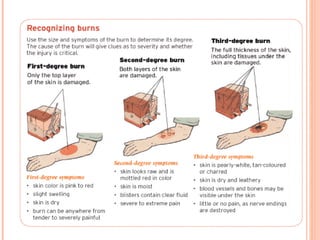
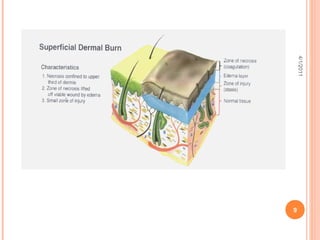
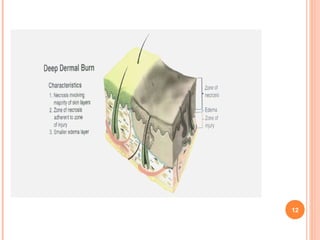
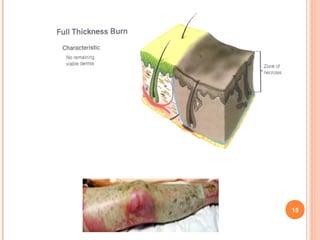
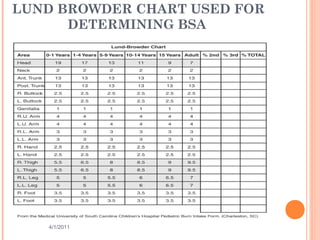
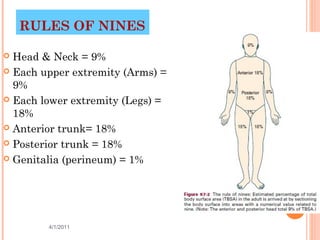
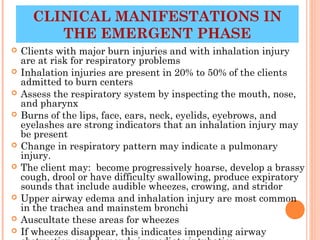
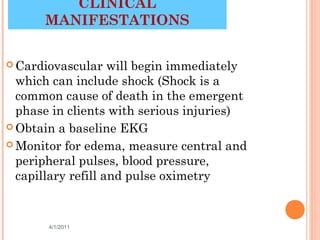
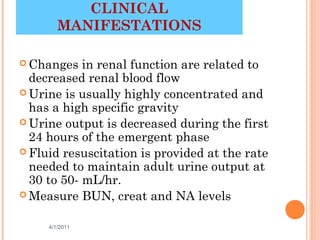
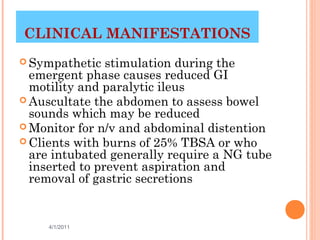
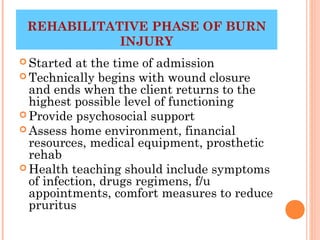
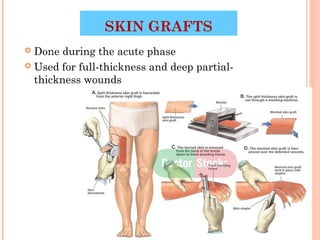
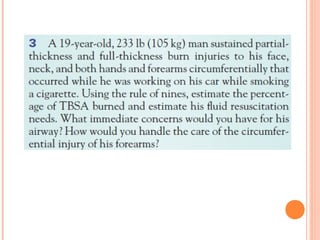
This document discusses different types of burns including thermal, chemical, electrical, and radiation burns. It describes how burns are assessed based on depth and extent of body surface area involved. First, second, and third degree burns are defined. Fluid imbalances that can occur with burns are also outlined. The phases of burn injuries - emergent, acute, and rehabilitative - are summarized along with goals, nursing interventions, and considerations for each phase. Wound care including dressing changes and skin grafting is also covered at a high level.