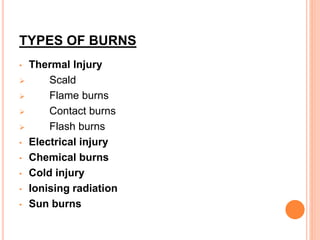
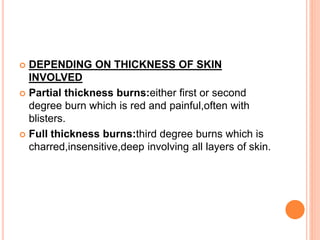
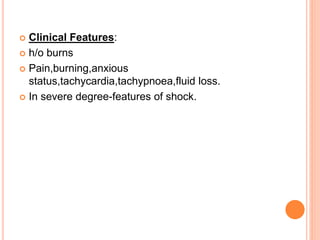
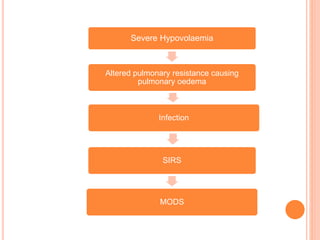
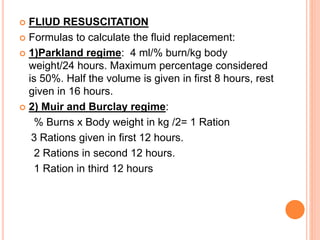
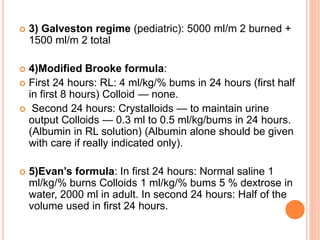
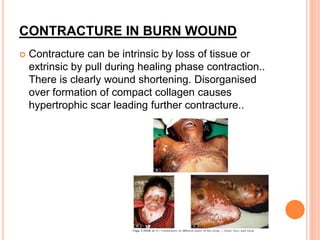
This document discusses types, classification, assessment, pathophysiology, effects, management, and complications of burns. It covers topics such as thermal, electrical, chemical, and inhalation burns. Burns are classified based on thickness of skin involvement from first to fourth degree. Assessment involves determining burn size using the Rule of Nines or Lund and Browder chart. Management consists of fluid resuscitation, wound care, surgery, and treatment of complications like infection and contractures.