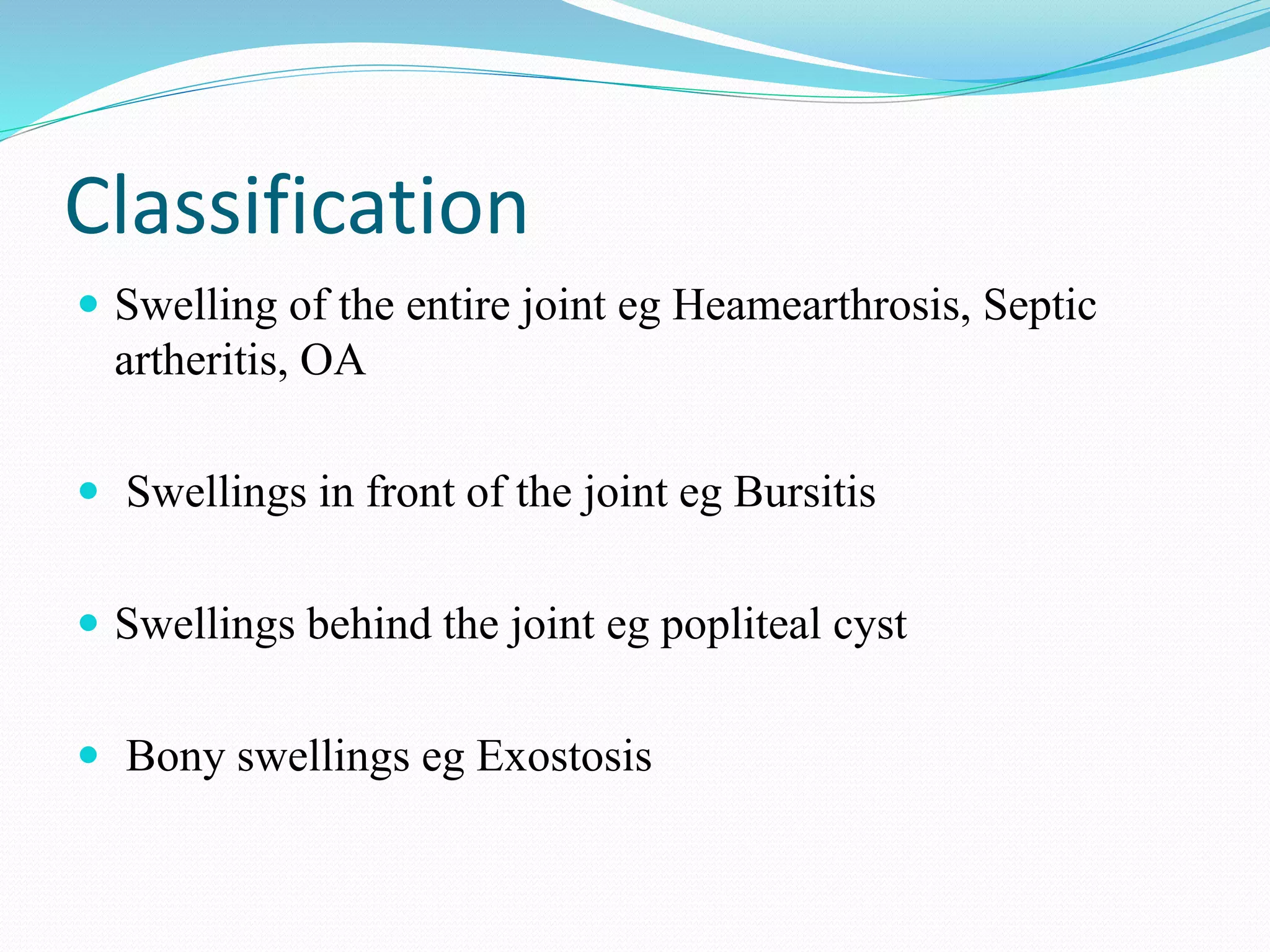
The document discusses gross knee swelling, which can have many causes including trauma, infection, osteoarthritis, rheumatoid arthritis, and hemophilia. It classifies different types of knee swellings and provides a brief anatomy of the knee joint. For evaluation and management, the document recommends history, physical exam, imaging tests like x-ray and MRI, joint aspiration/biopsy, and treatments tailored to the underlying cause, such as antibiotics for infection, joint replacement for arthritis, or splinting and factor replacement for hemophilia. Precise diagnosis of the cause is important for successful management of gross knee swelling.