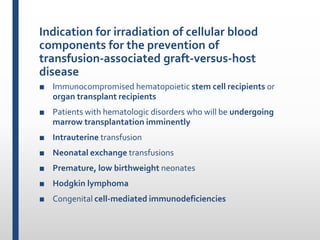
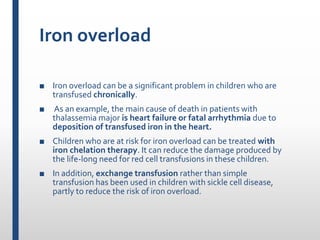
This document discusses various complications that can occur from red blood cell transfusions in children. It outlines several types of transfusion reactions including acute and delayed hemolytic reactions, febrile reactions, allergic reactions, transfusion-associated lung injury, infection, circulatory overload, metabolic toxicity, graft-versus-host disease, and iron overload. For each complication, it describes the clinical manifestations, diagnostic evaluation, and treatment approach.