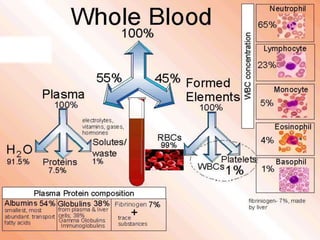
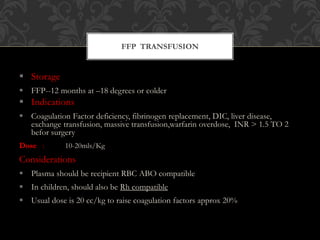
This document discusses blood component transfusion. It defines blood components as any therapeutic substance prepared from human blood, including whole blood, red blood cells, platelets, plasma, cryoprecipitate, and growth factors. It describes how whole blood is separated into components through centrifugation. It provides indications, storage requirements, and dosages for transfusing various blood components in pediatric patients. Potential complications of transfusion like acute reactions, late infections, and iron overload are also summarized. The document concludes with SKMCH&RC transfusion protocols.