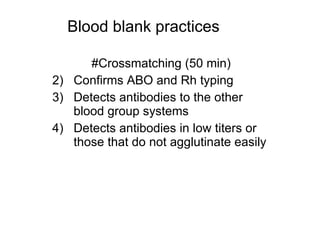
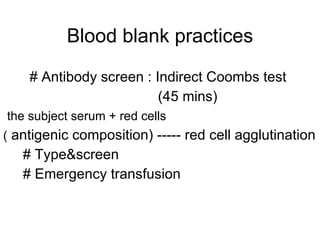
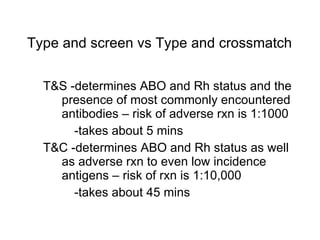
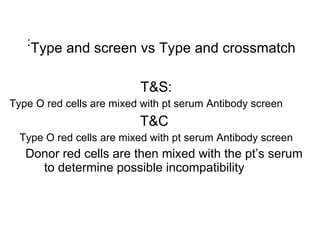
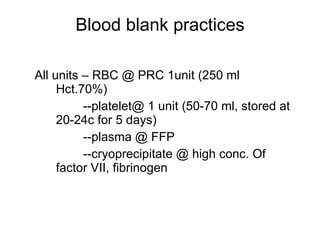
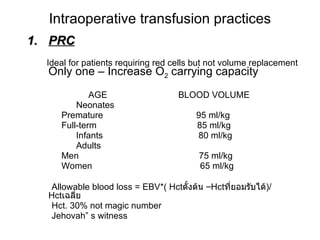
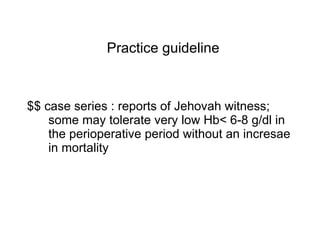
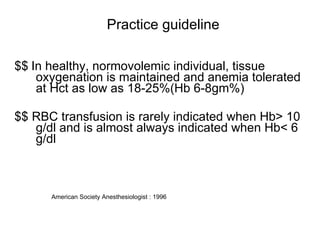
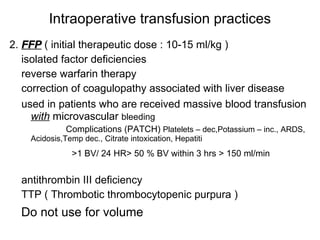
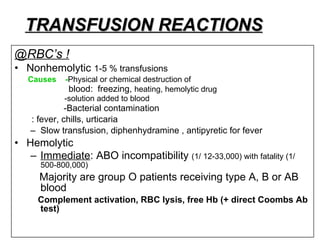
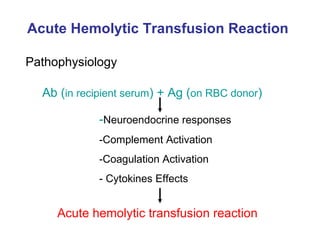
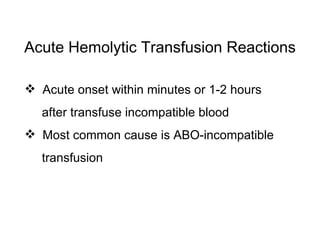
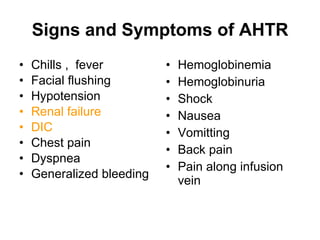
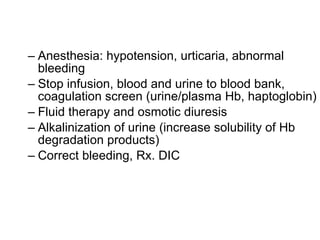
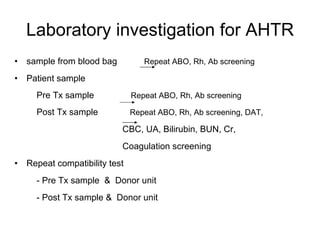
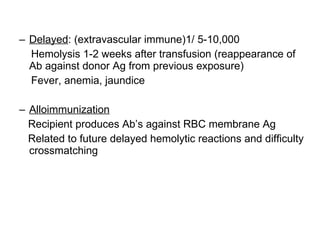
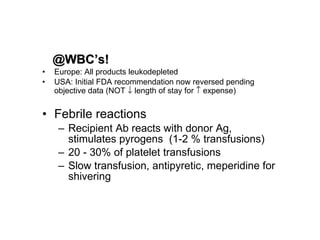
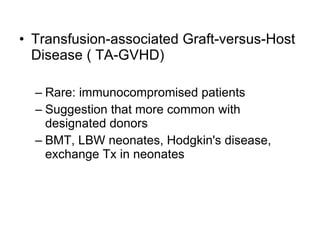
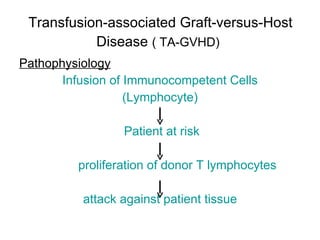
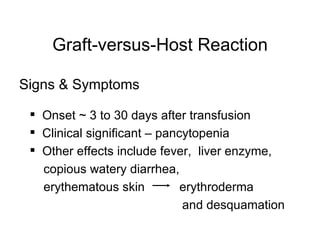
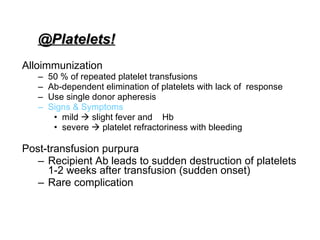
Blood transfusion practices involve determining a patient's blood type and screening for antibodies to reduce risks of transfusion reactions like hemolytic reactions. Key indications for transfusion include maintaining hemoglobin above 6-8 g/dL and allowing blood loss within established volumes. Complications can be minimized through proper blood type matching, leukoreduction, and following guidelines for transfusion thresholds and volumes.