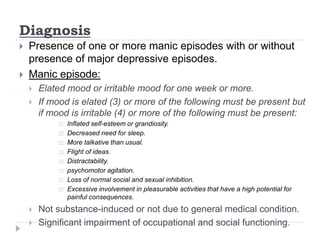
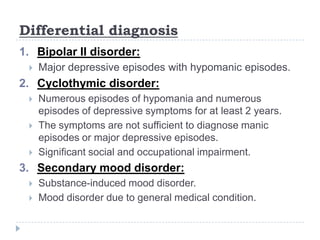
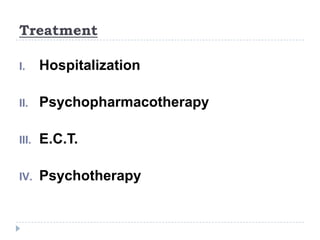
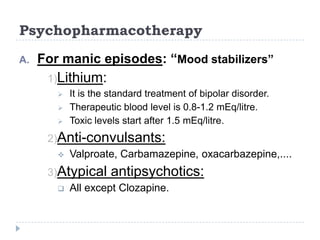
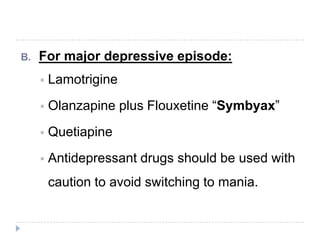
Bipolar I disorder is characterized by one or more manic episodes, with or without major depressive episodes. The lifetime prevalence is 0.4-1.6% and is highly genetic, with a 90% prevalence in monozygotic twins of patients. Diagnosis requires a manic episode lasting at least one week with inflated self-esteem and decreased need for sleep, plus additional symptoms. Treatment involves hospitalization, psychopharmacotherapy including mood stabilizers like lithium, and psychotherapy.