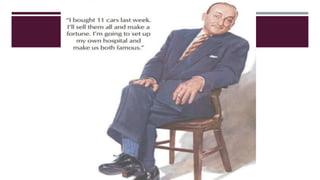
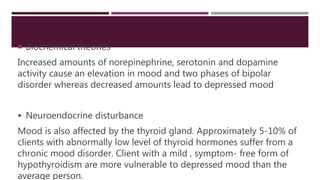
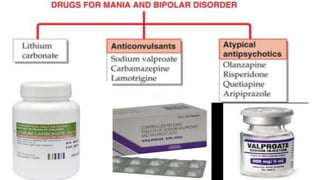
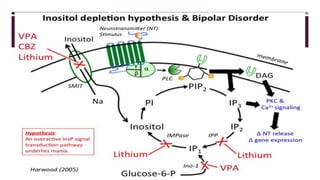
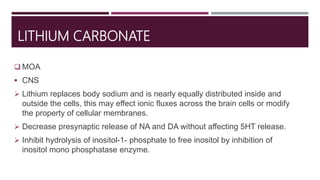
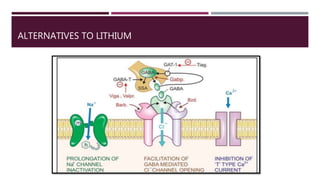
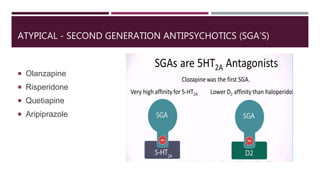
This document discusses mania, which is a mental disorder characterized by periods of euphoria and overactivity. It is commonly associated with bipolar disorder. The document outlines the stages and symptoms of mania and describes the biological, psychological, and social causes. It then discusses the mechanisms and side effects of lithium carbonate and some alternative treatments for mania including sodium valproate, carbamazepine, lamotrigine, and atypical antipsychotics.