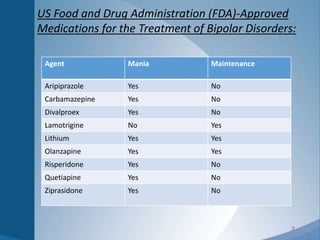
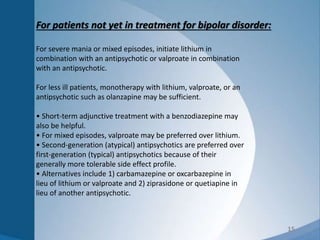
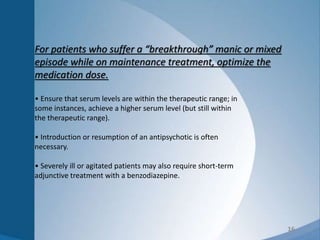
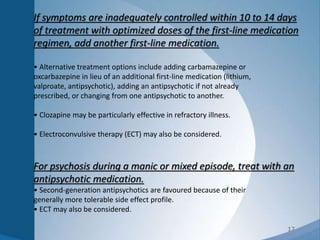
1) The document discusses pharmacological management of bipolar disorder. It outlines treatment options for acute manic or mixed episodes, including lithium, valproate, and antipsychotics.
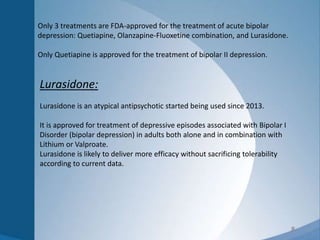
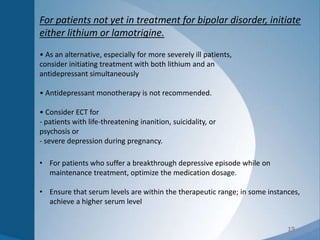
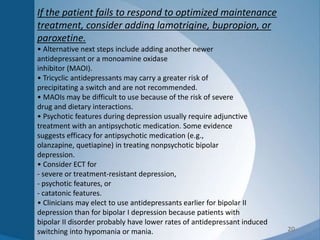
2) It also discusses treatment for acute depression, with a goal of achieving remission without precipitating a manic episode. Medications approved for bipolar depression include quetiapine, olanzapine-fluoxetine combination, and lurasidone.
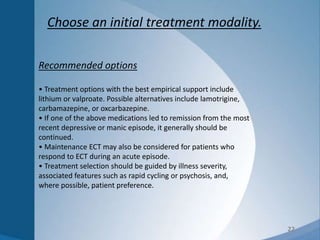
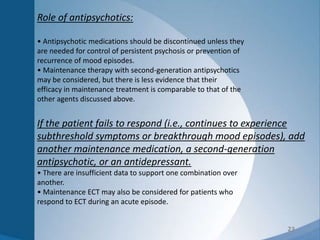
3) Maintenance treatment options are also outlined, including lithium, lamotrigine, lurasidone, and several antipsychotics as FDA-approved medications for treating bipolar disorder.
![4
Bipolar II Disorder:
The diagnostic criteria for bipolar II disorder is characterized by depressive
episodes and hypomanic episodes during the course of the disorder, but the
episodes of manic-like symptoms do not quite meet the diagnostic criteria for a
full manic syndrome.
Evidence also indicates that patients with bipolar II disorder are at greater risk of
both attempting and completing suicide than patients with bipolar I disorder and
major depressive disorder.
Manic episodes clearly precipitated by antidepressant treatment (e.g.,
pharmacotherapy, electroconvulsive therapy [ECT]) indicate bipolar III disorder.](https://image.slidesharecdn.com/bipolardisorder-150818065919-lva1-app6892/85/Bipolar-disorder-4-320.jpg)