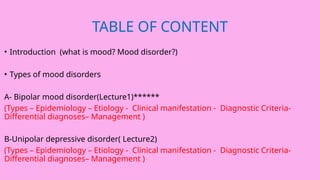
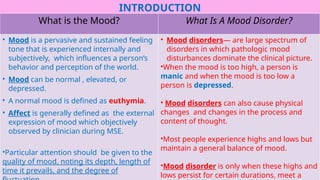
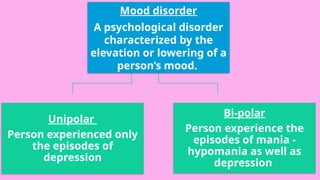
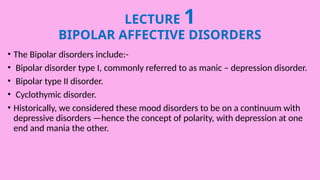
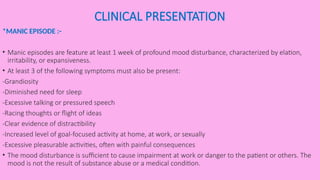
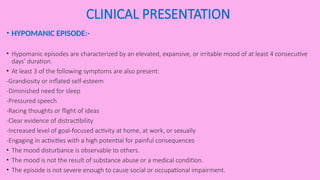
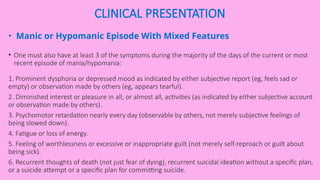
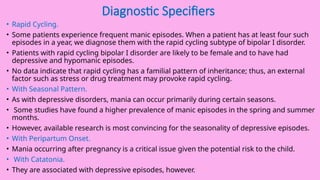
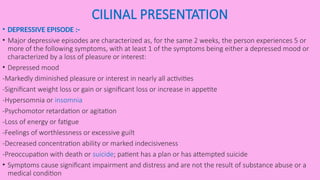
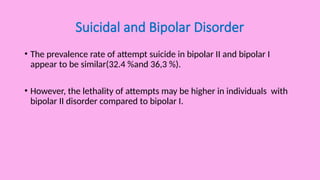
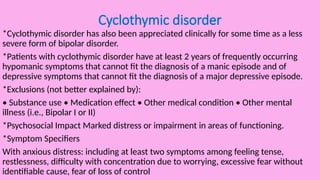
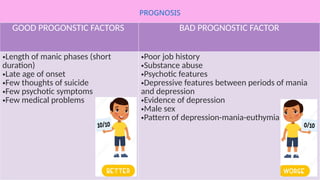
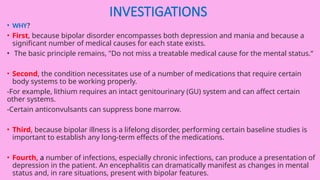
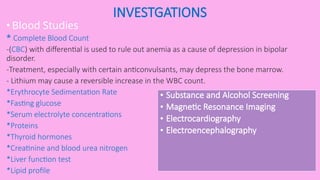
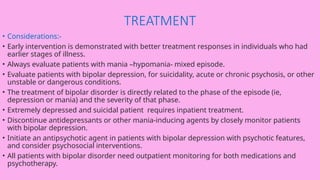
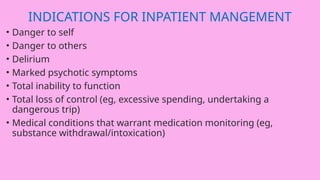
The document is a comprehensive lecture on mood disorders, focusing on bipolar and unipolar depressive disorders, detailing their definitions, types, epidemiology, etiology, clinical presentations, and management strategies. It explores the biological, psychodynamic, and environmental factors influencing these disorders and discusses diagnostic criteria, differential diagnoses, and treatment options. Additionally, it highlights the need for proper investigations and monitoring due to the lifelong nature of bipolar disorder.