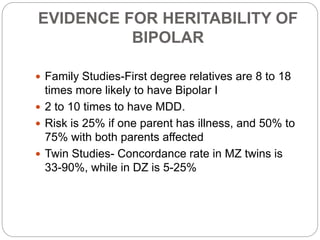
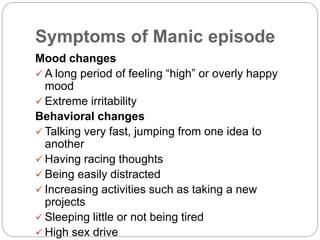
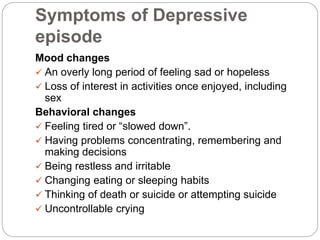
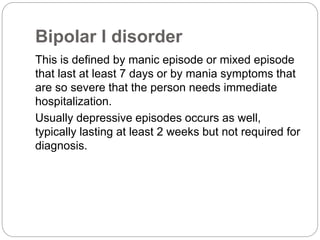
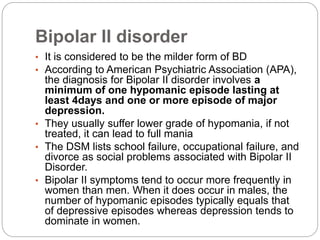
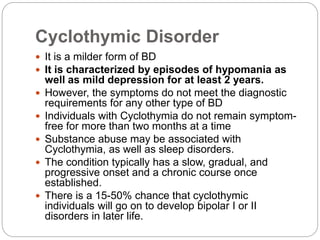
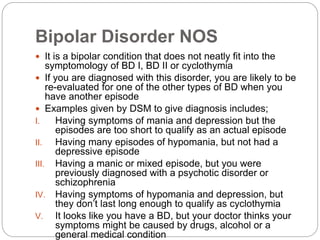
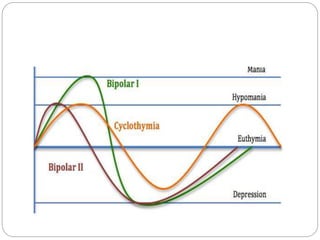
Bipolar disorder is a mental illness characterized by extreme mood swings from mania to depression. It affects about 0.6-0.9% of the population. While the exact cause is unknown, it is believed to involve genetic and environmental factors. Symptoms include changes in mood and behavior during manic, depressive, hypomanic or mixed episodes. There are several types of bipolar disorder that are diagnosed based on the severity and length of episodes. Treatment involves medications, psychotherapy, and in some cases electroconvulsive therapy, with the goals of managing mood swings and preventing relapse. Proper long-term treatment can help people with bipolar disorder lead productive lives.