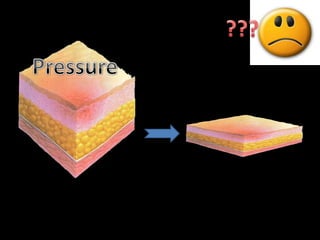
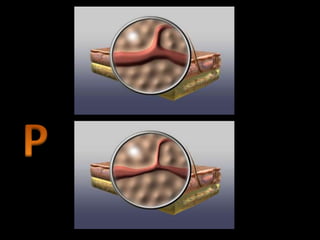
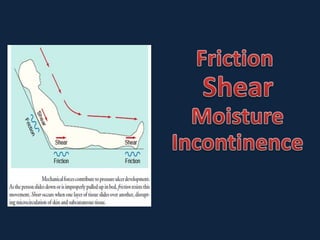
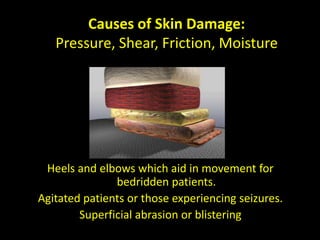
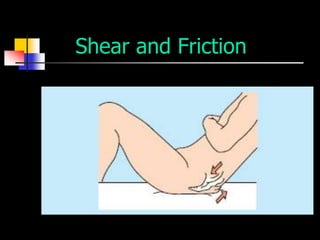
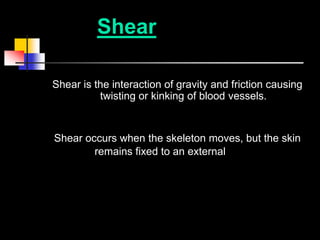
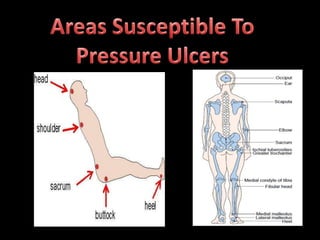
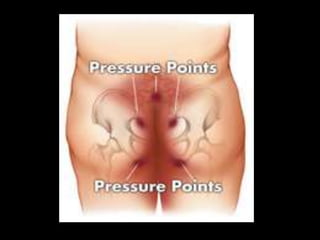
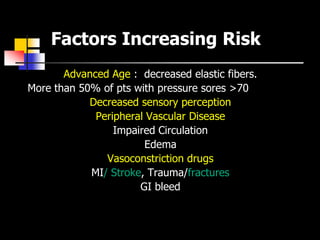
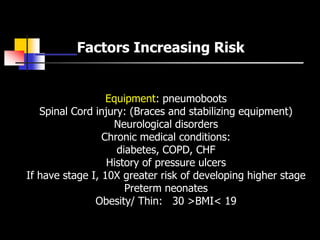
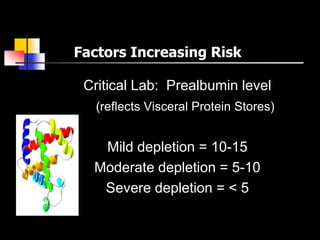
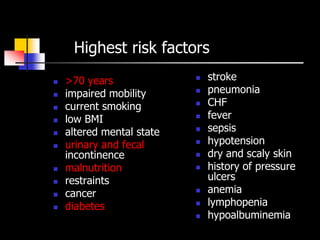
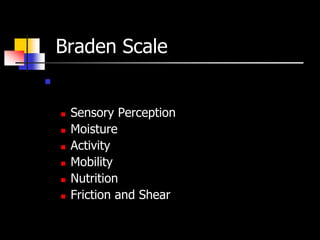
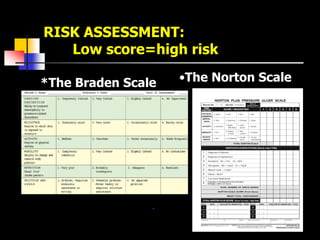
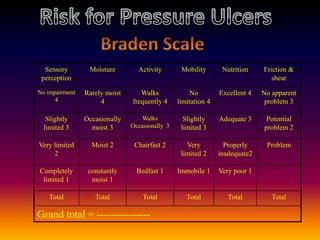
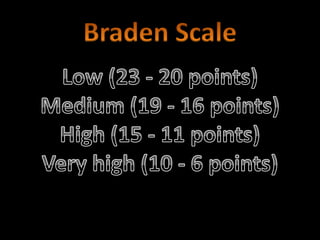
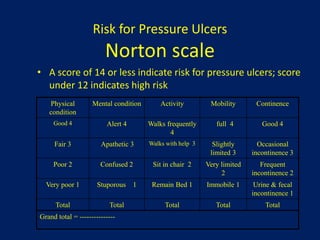
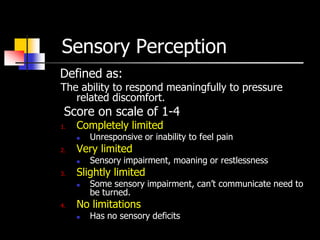
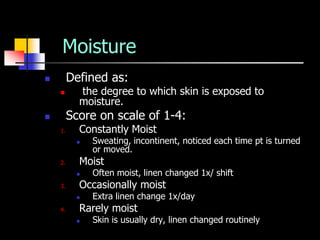
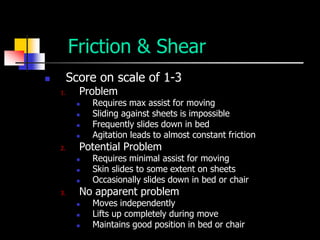
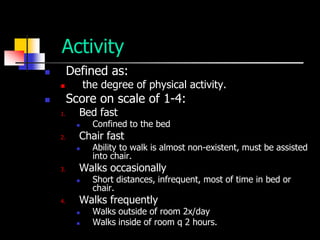
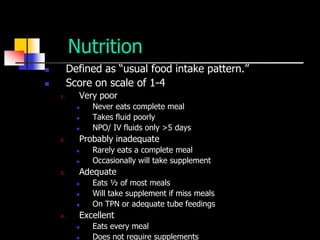
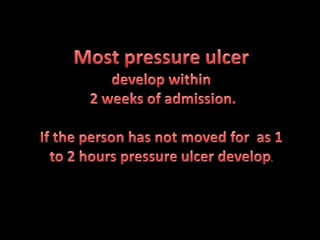
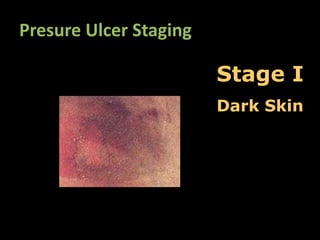
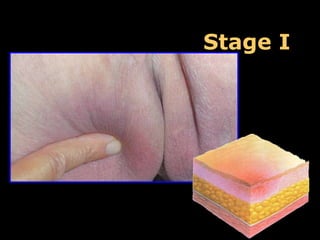
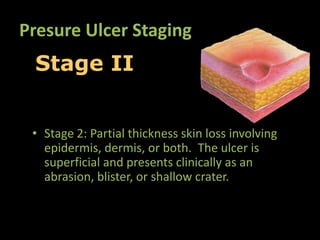
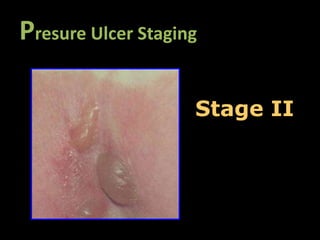
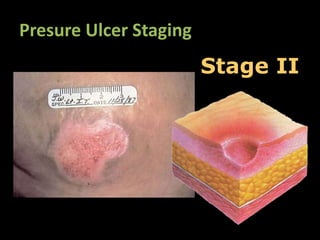
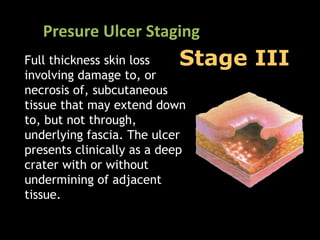
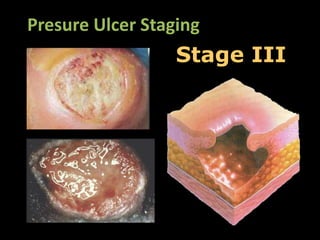
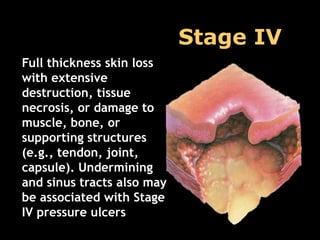
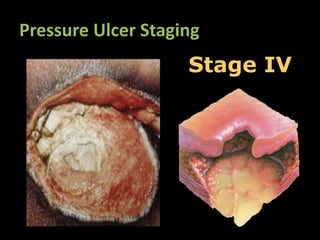
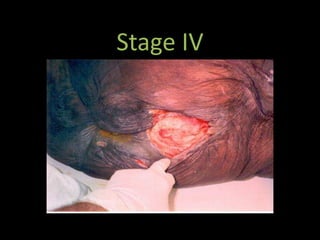
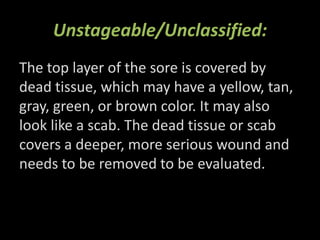
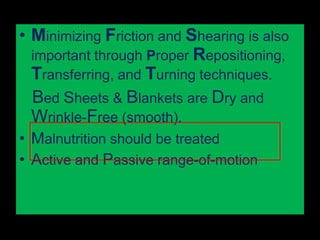
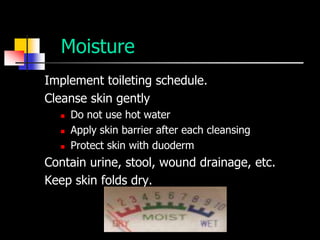
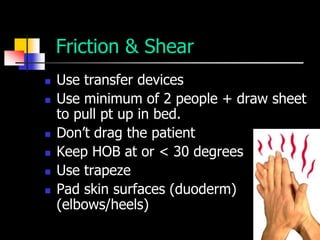
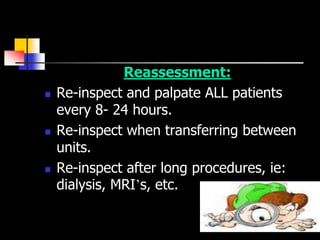
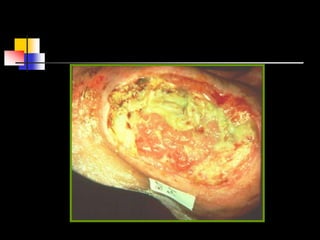
This document discusses various factors that can cause skin damage, including pressure, shear, friction, and moisture. It provides examples of how shear and friction can damage skin, such as when pulling a patient up in bed or during a slide transfer. Risk factors for skin breakdown are also outlined, including age, impaired mobility, nutrition status, and medical conditions. Tools for assessing risk like the Braden Scale are presented. Stages of pressure ulcers from I to IV are defined along with images. The importance of regular skin assessment is emphasized.