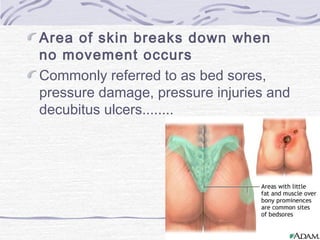
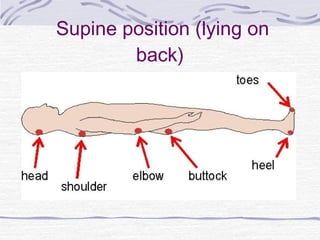
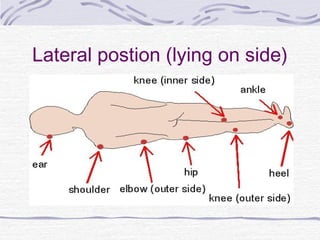
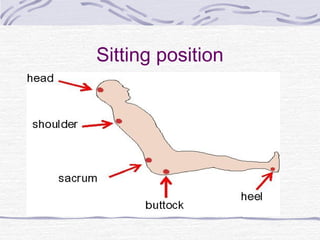
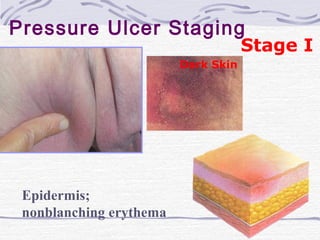
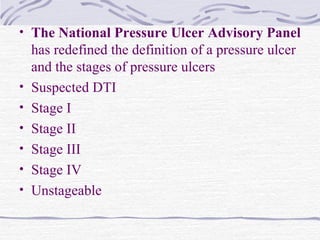
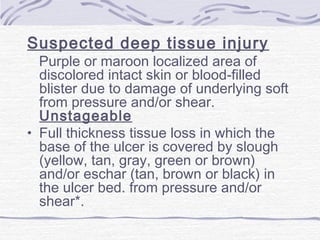
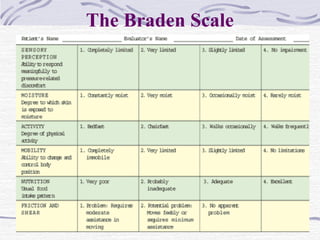
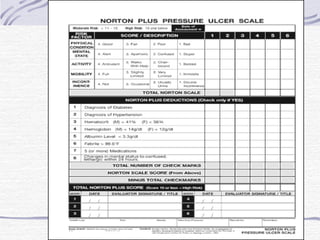
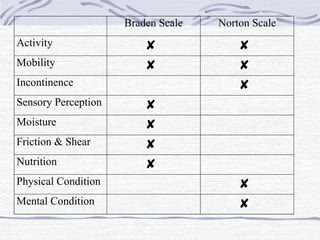
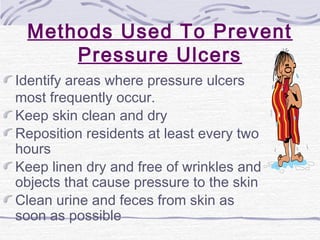
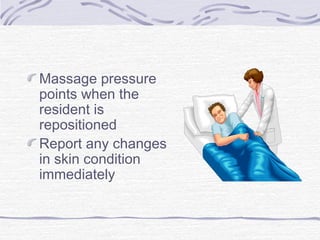
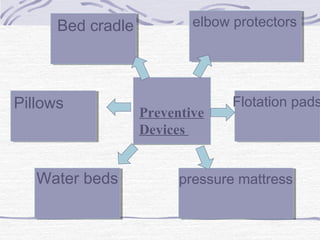
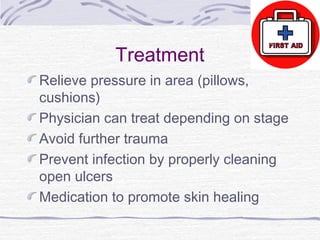
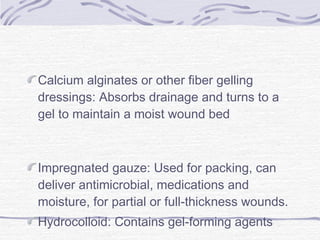
Pressure ulcers, also known as bedsores, develop when skin and underlying tissue is damaged due to prolonged pressure, friction, or moisture. They typically form over bony areas of the body. Factors that increase risk include immobility, incontinence, poor nutrition, aging, and chronic diseases. Pressure ulcers are staged from I to IV based on the depth of tissue damage. Prevention focuses on relieving pressure through repositioning, special beds and cushions, and keeping skin clean and dry. Treatment may include dressings, debridement, and medications to promote healing.