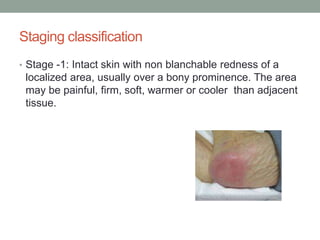
Pressure sores, also known as decubitus ulcers or bed sores, are localized skin injuries caused by prolonged pressure, friction, or shearing forces that impair blood flow. They commonly form over bony areas of immobilized patients and cost health systems billions annually to treat. Prevention focuses on reducing pressure, moisture, and shearing through frequent repositioning, skin care, nutrition, and devices like air mattresses. Pressure sores are staged from 1 to 4 based on tissue depth involvement and managed accordingly through cleaning, debridement, dressings, and sometimes antibiotics.