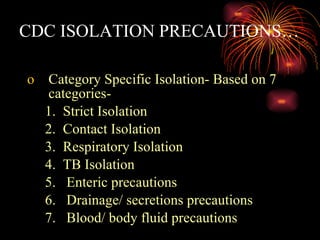
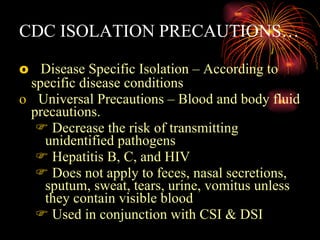
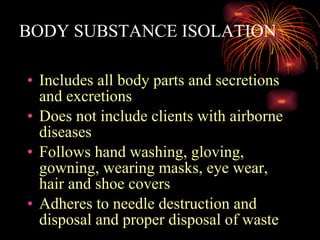
Medical asepsis refers to practices that limit the transmission of disease-causing microorganisms between patients and their environment. Key methods of medical asepsis include isolation precautions, hand washing, use of protective equipment like gowns and gloves, disinfection of surfaces and equipment, and maintaining staff and patient health and hygiene. Isolation systems used in healthcare facilities include category-specific isolation, disease-specific isolation, and universal precautions based on CDC guidelines.