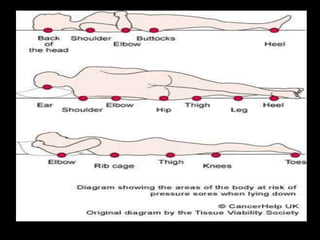
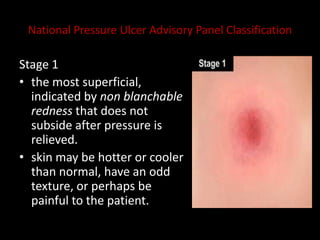
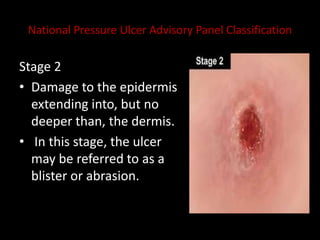
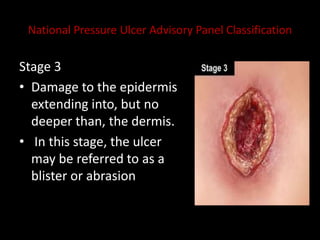
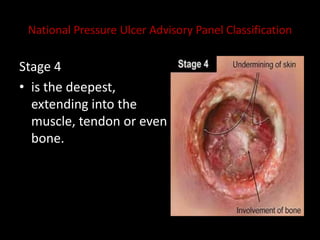
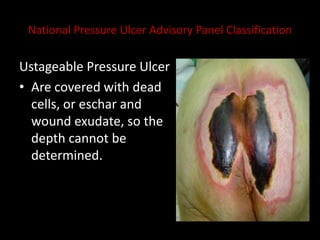
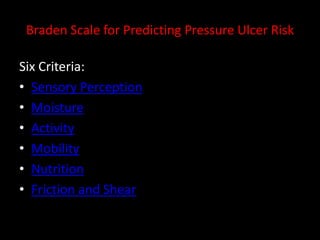
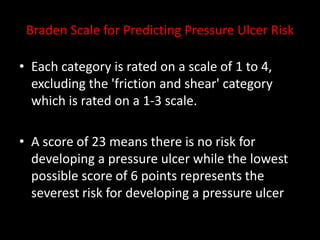
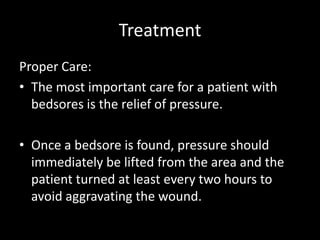
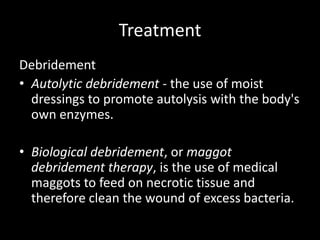
This document discusses bed sores (also known as pressure ulcers or decubitus ulcers), including their causes, risk factors, common areas, stages, assessment using the Braden scale, and treatment. Prolonged pressure on bony areas can lead to reduced blood flow and skin breakdown. The sacrum, elbows, knees, and ankles are most common. Risk increases with age, incontinence, poor nutrition, diabetes, and smoking. Bedsores are caused by pressure, shear forces, and friction. They are classified in stages based on depth of tissue damage. Treatment focuses on relieving pressure and proper wound care like debridement and dressing.