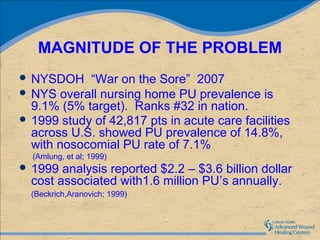
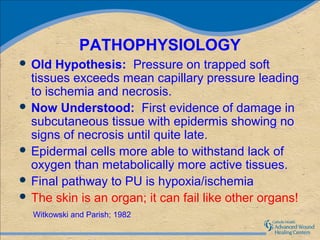
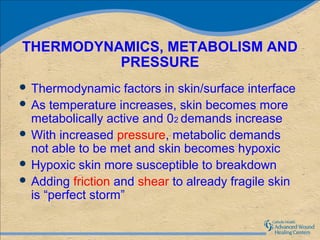
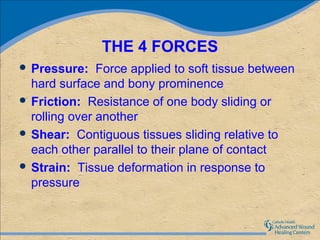
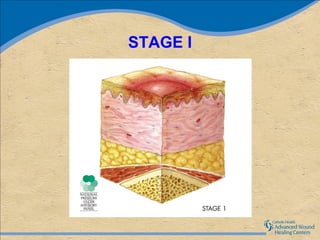
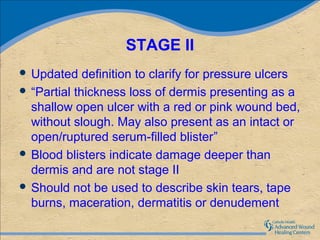
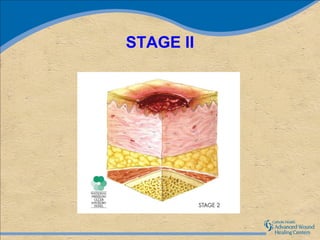
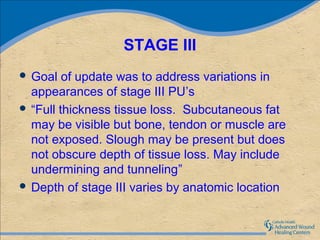
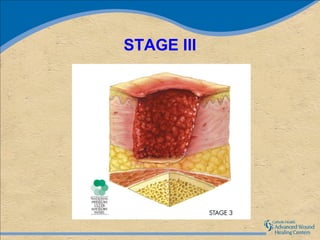
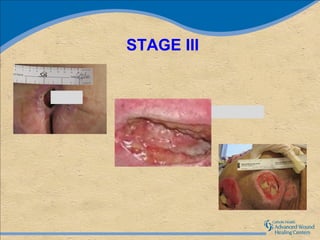
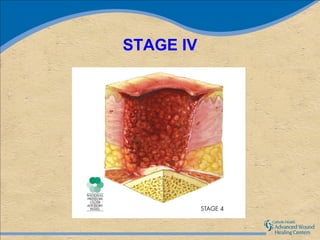
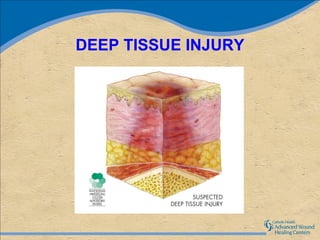
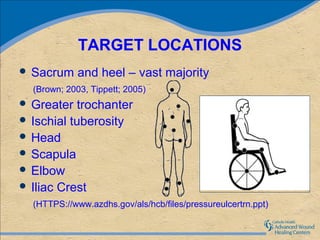
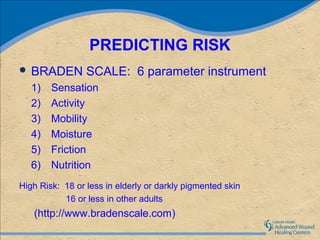
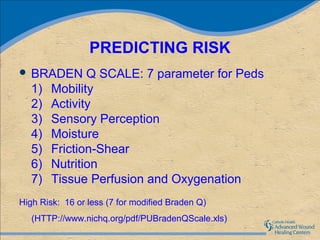
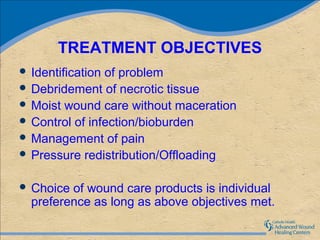
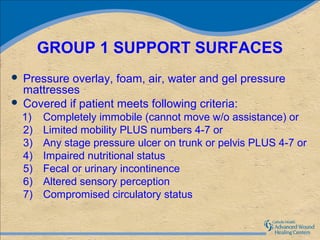
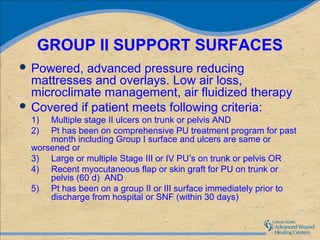
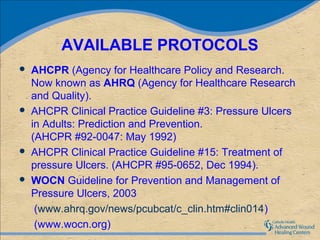
Pressure ulcers, also known as decubitus ulcers or bedsores, are localized injuries to the skin and underlying tissue that are usually caused by pressure over bony prominences. They are commonly seen in immobilized or bedridden patients and are associated with increased costs of care and risk of litigation. The Braden Scale is commonly used to assess pressure ulcer risk based on factors like mobility, sensation, moisture, activity, nutrition, and friction/shear. Treatment focuses on pressure redistribution through support surfaces, wound care including debridement and moist dressings, and managing pain and infection. Staging systems classify ulcers by depth of tissue damage from non-blanchable erythema to full thickness tissue loss.