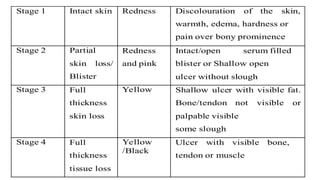
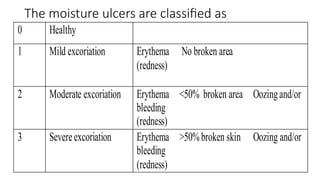
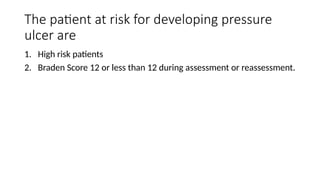
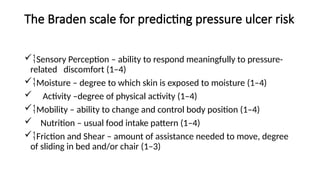
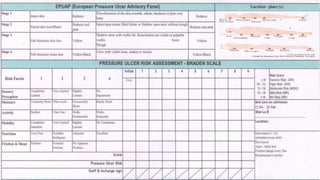
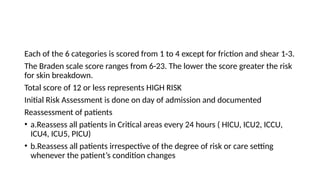
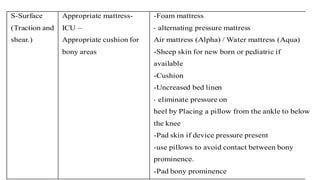
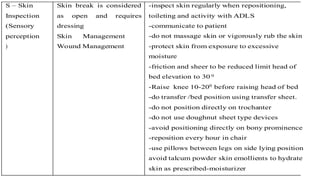
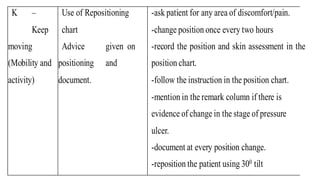
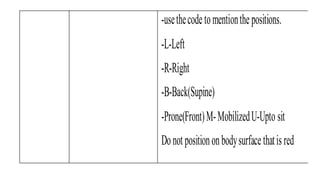
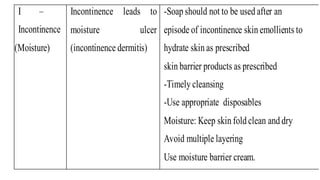
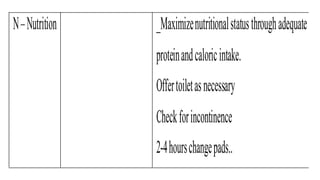
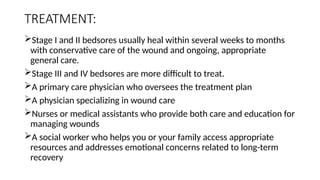
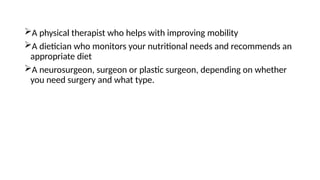
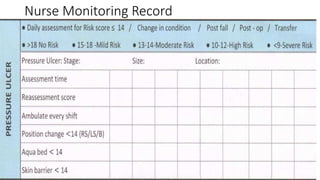
The document outlines the identification, prevention, and management of pressure ulcers, emphasizing the roles of healthcare staff in assessing and addressing risks. It details risk factors, patient assessment procedures using the Braden scale, and the SSKIN bundle for preventing pressure ulcers. Additionally, it highlights the importance of nutrition, regular repositioning, and appropriate wound care for effective treatment.