- IAD is skin damage caused by exposure to urine and/or stool, and is exacerbated by the use of absorbent containment products. It affects 5.6-50% of long-term care residents and 10.9-54% of incontinent hospital patients.
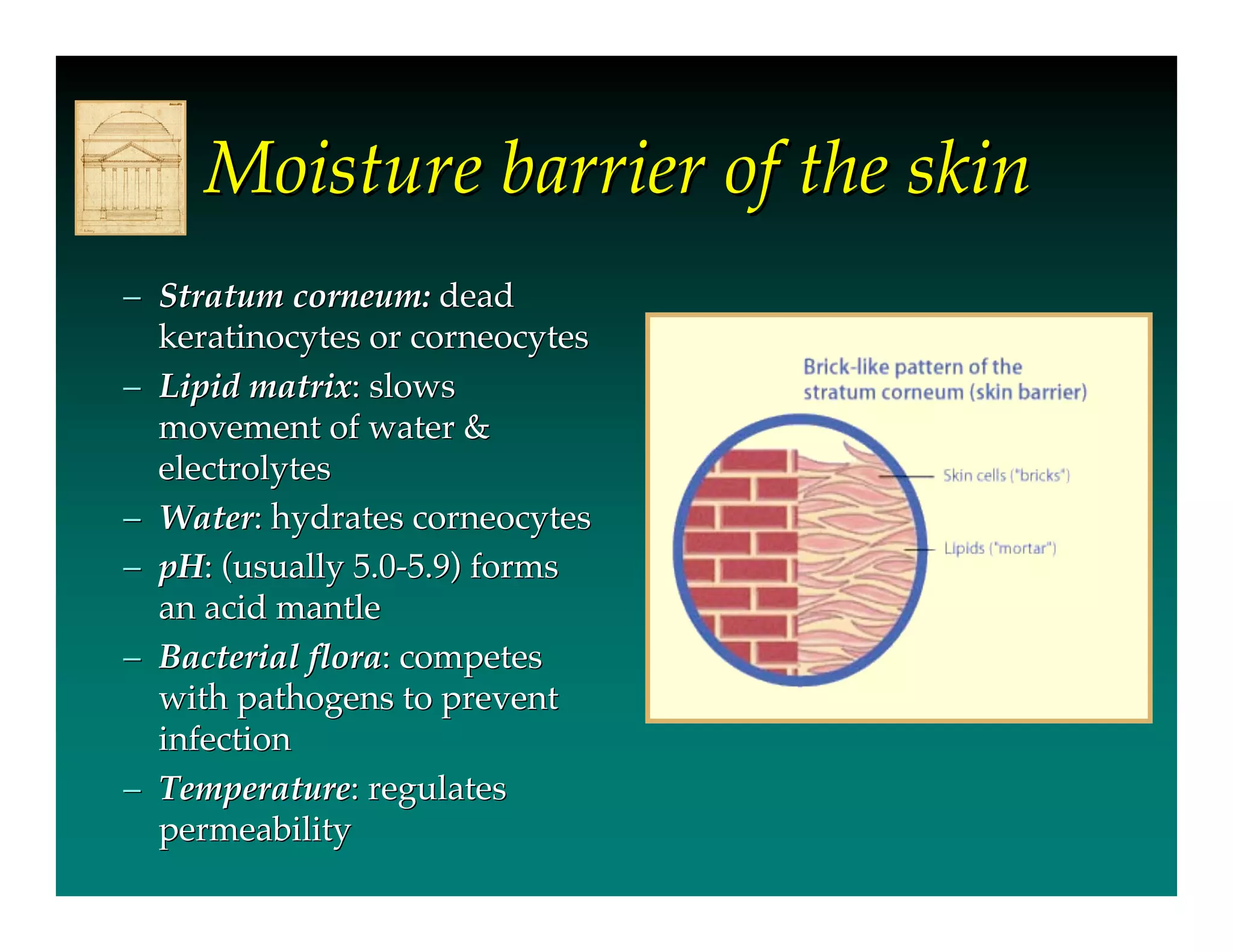
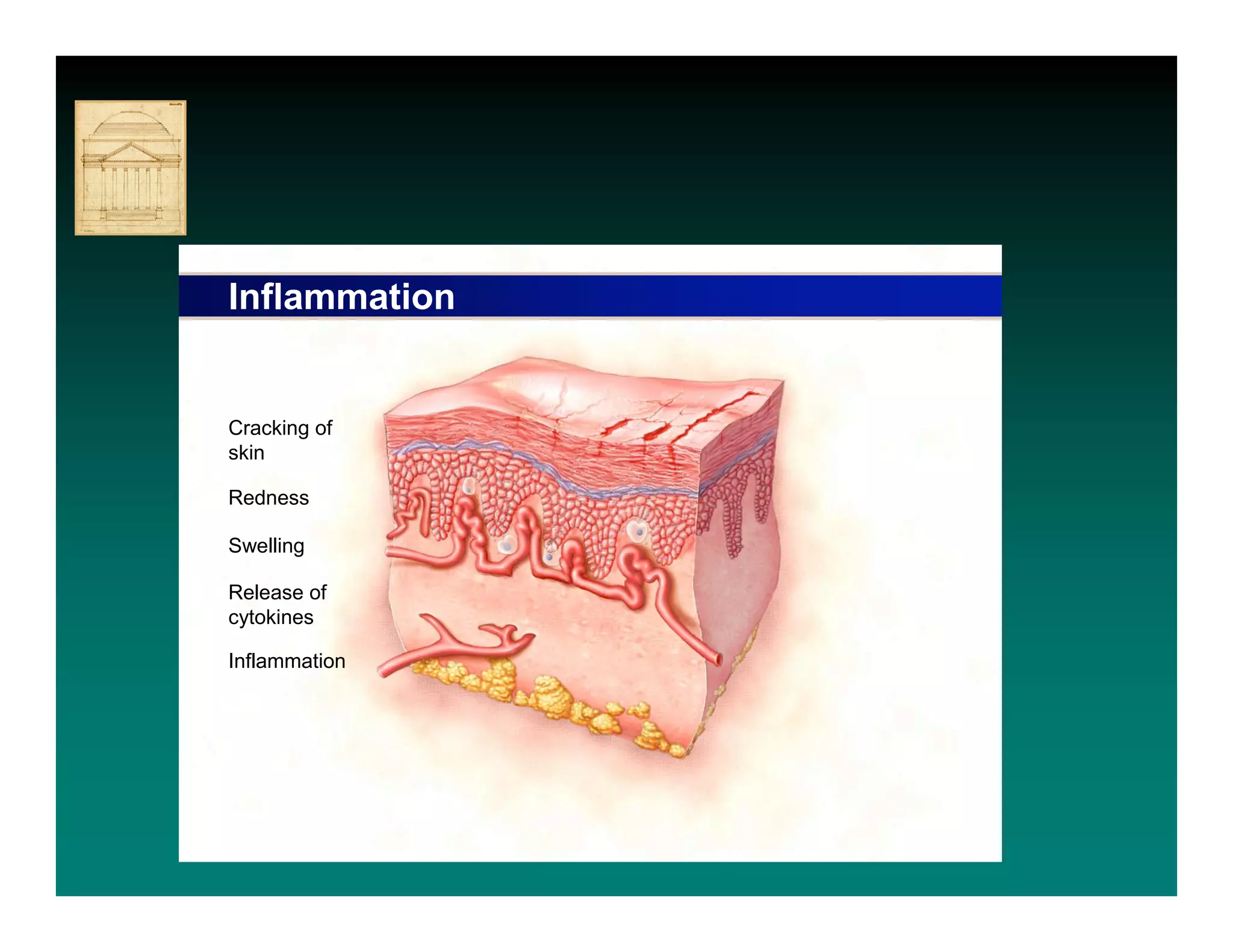
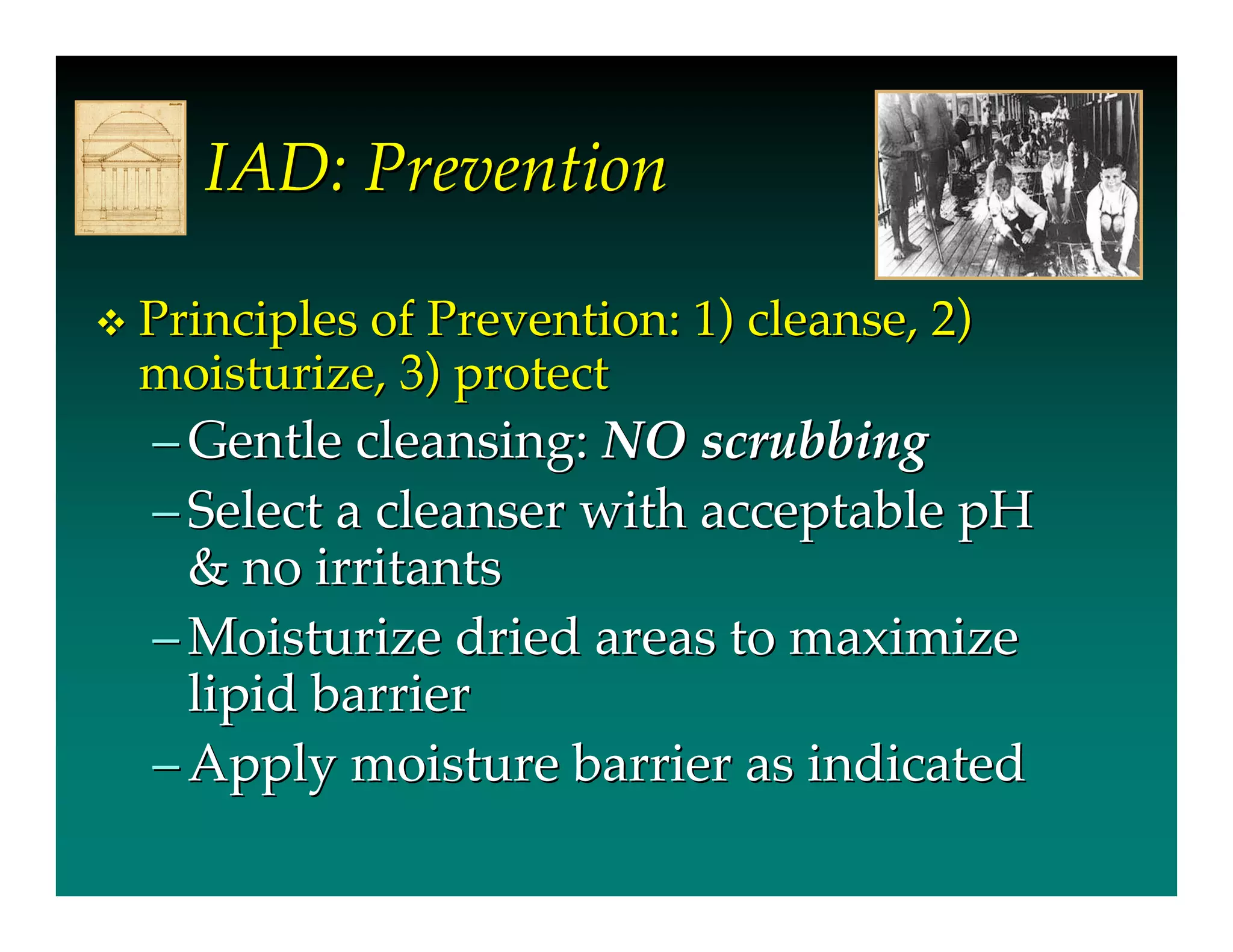
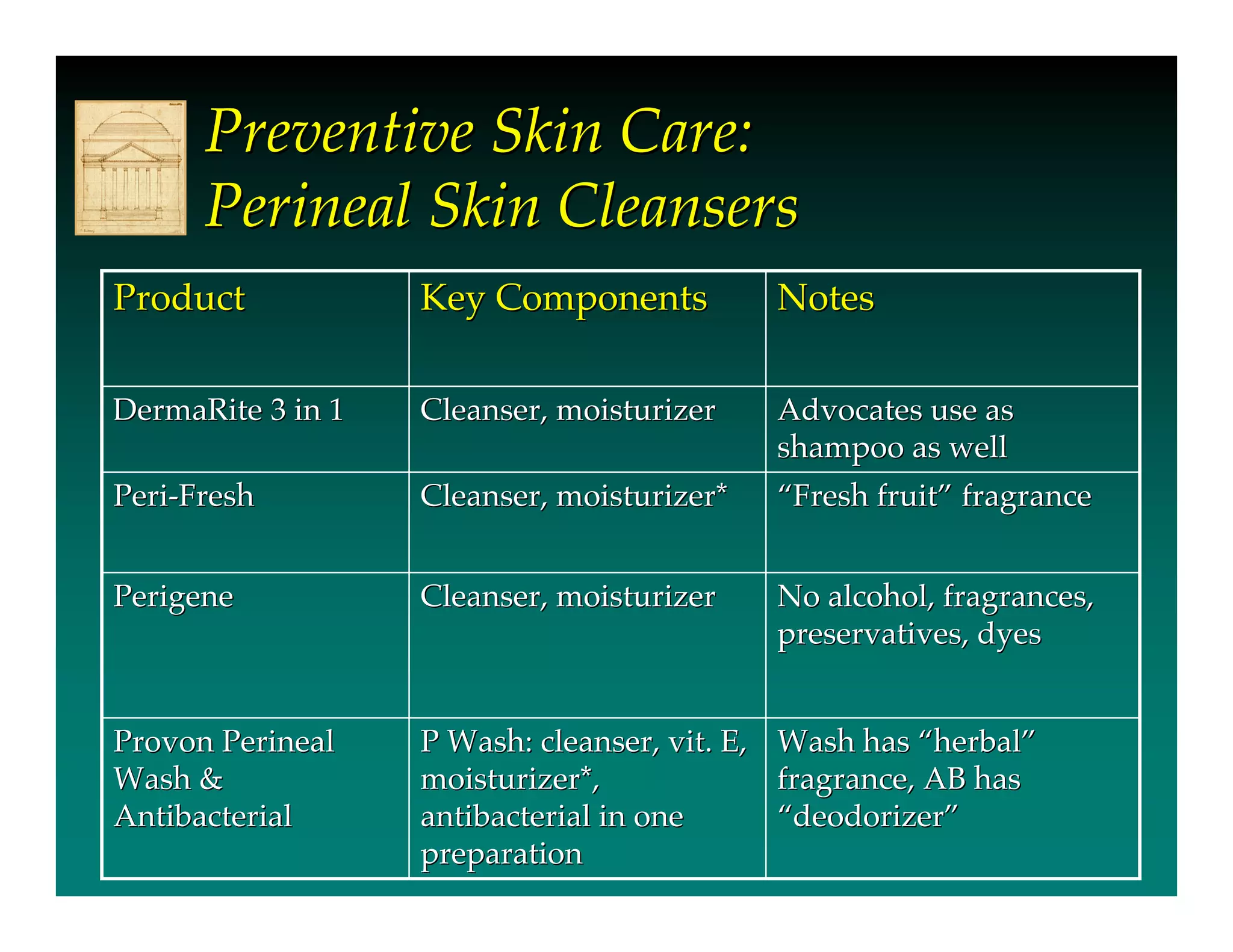
- Urine and stool impact the skin's moisture barrier, increasing pH and promoting bacterial/fungal growth. Absorbent products further overhydrate the skin.
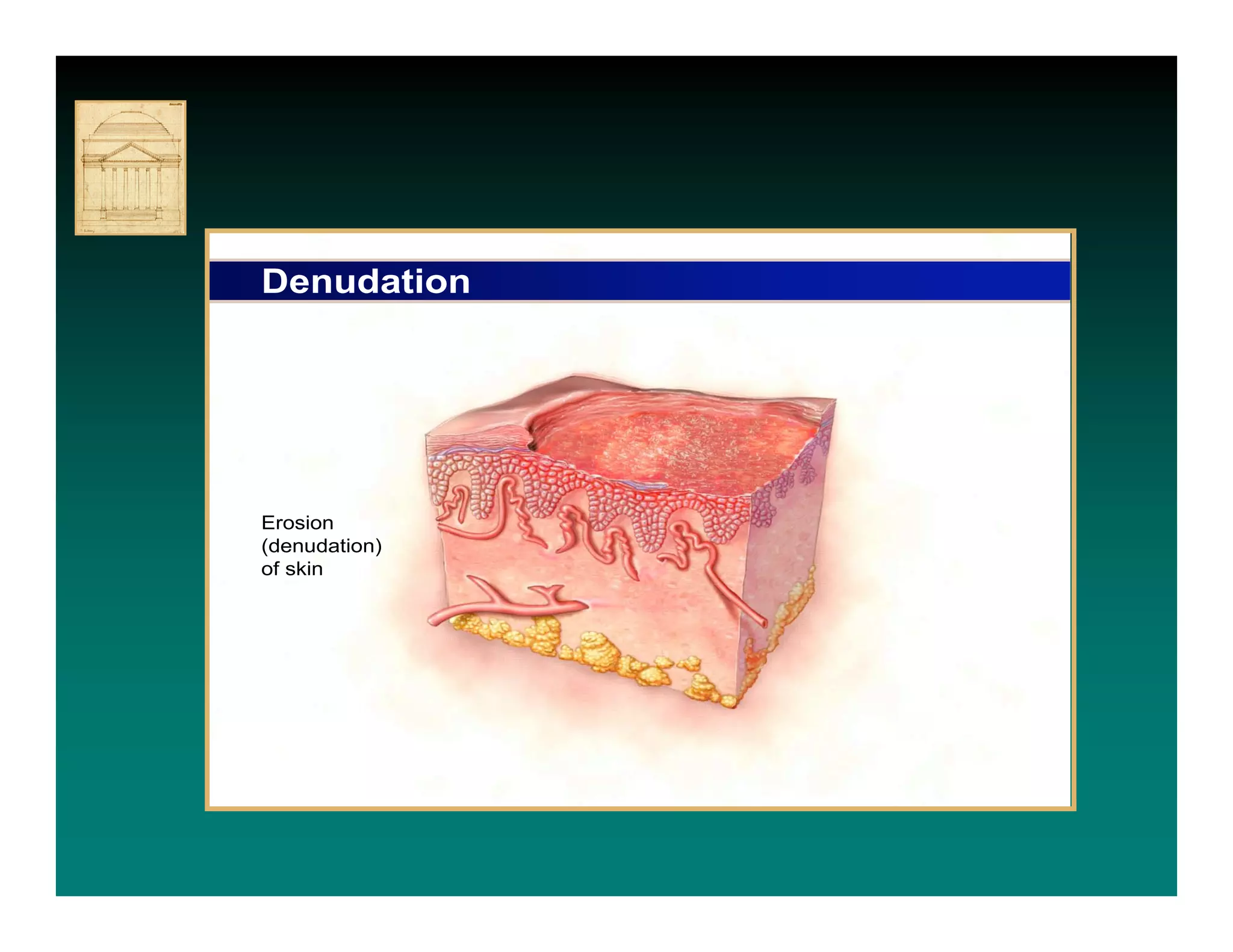
- IAD is diagnosed by inspecting the skin for redness,