The skeletal system performs several critical functions:
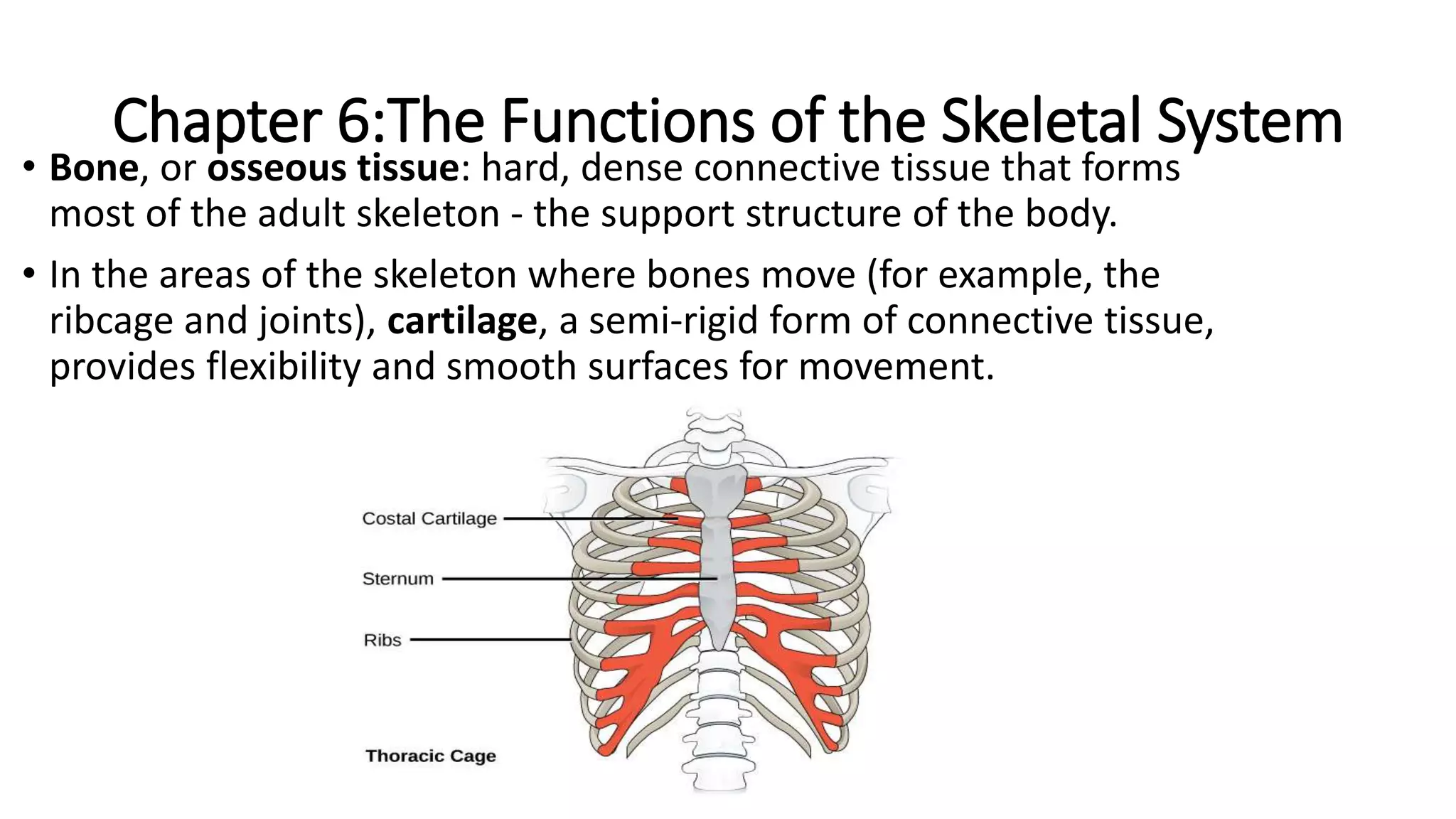
1. It supports the body and facilitates movement by providing attachment points for muscles and acting as levers.
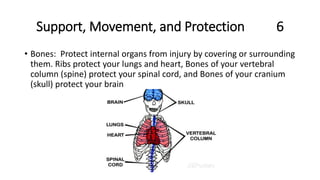
2. Bones protect internal organs such as the lungs, heart, and brain.
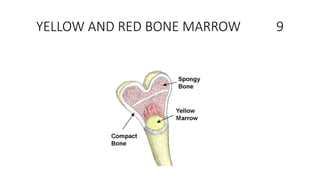
3. The skeletal system stores and releases minerals and produces blood cells. Bones store minerals like calcium and release them when needed, and bone marrow produces red blood cells, white blood cells, and platelets.