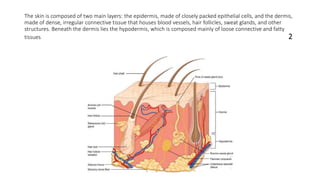
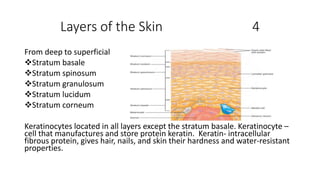
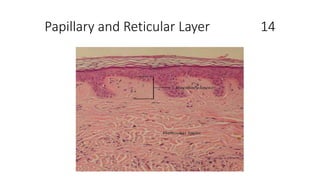
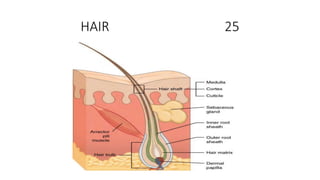
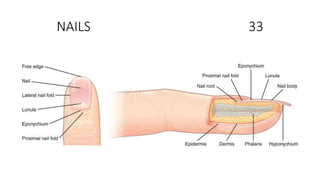
The document summarizes key aspects of the integumentary system, including the skin and its layers, hair, nails, and other accessory structures. It describes the three main layers of the skin - the epidermis, dermis, and hypodermis - and provides details on the layers within the epidermis including the stratum basale, stratum spinosum, stratum granulosum, stratum lucidum, and stratum corneum. It also discusses hair structure, growth cycles, color, nails, glands, and other topics.