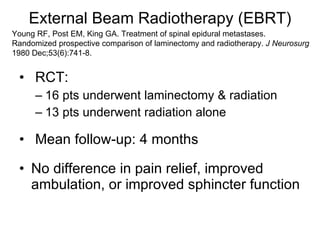
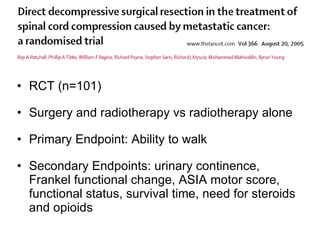
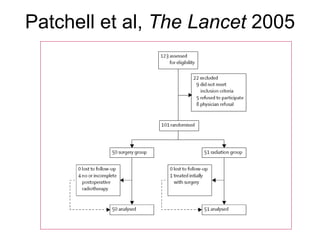
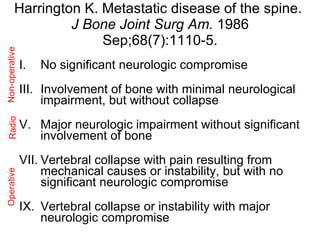
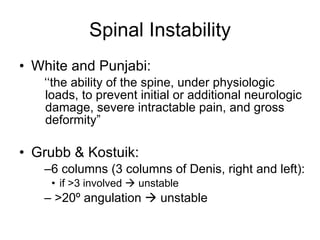
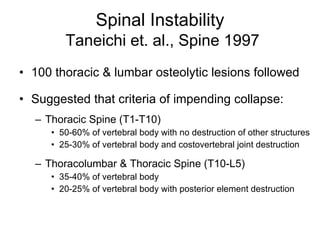
The document provides an extensive overview of spinal metastases, highlighting their epidemiology, pathophysiology, clinical presentation, and treatment options. It examines the role of spine surgeons in diagnosing and managing these conditions, discussing various therapeutic strategies including surgery, radiotherapy, and pharmacological approaches such as bisphosphonates. The document emphasizes the need for a multidisciplinary approach to maximize patient outcomes and improve quality of life.