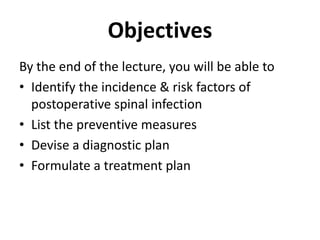
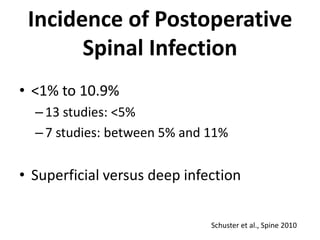
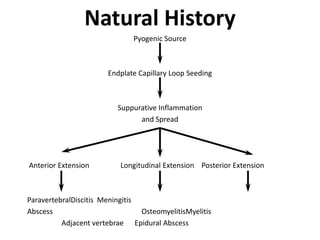
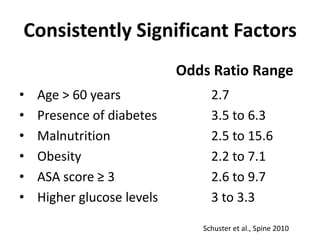
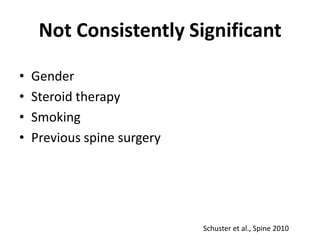
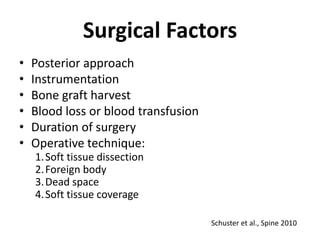
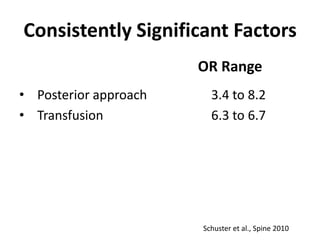
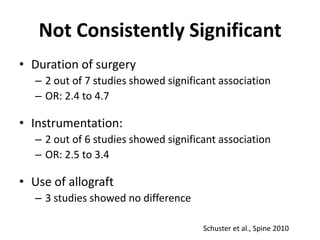
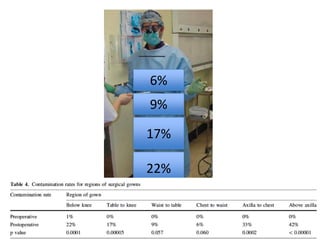
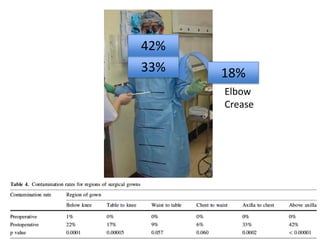
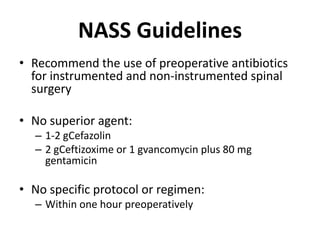
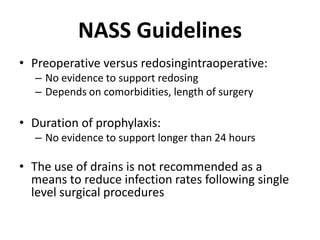
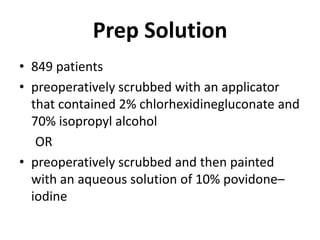
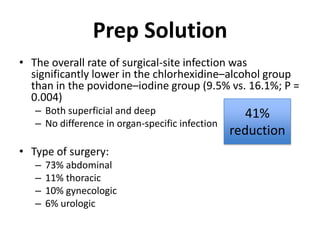
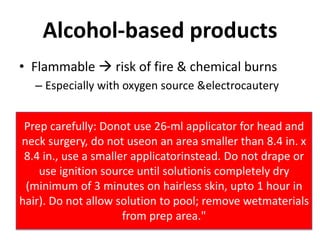
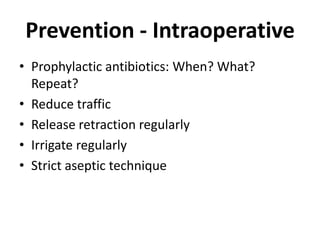
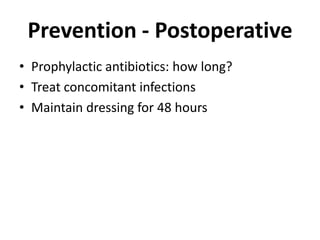
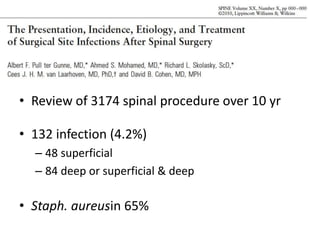
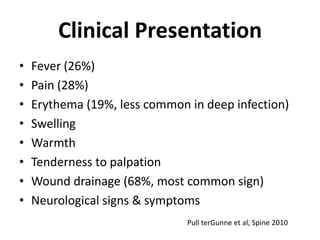
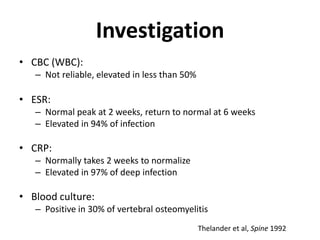
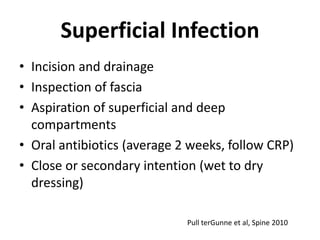
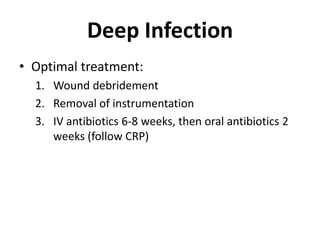
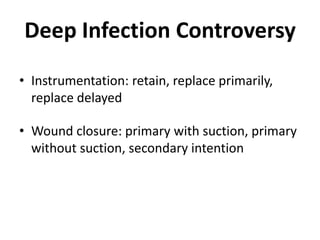
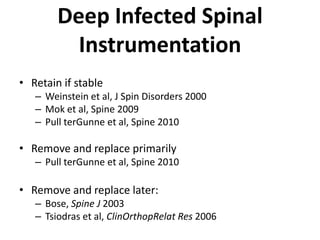
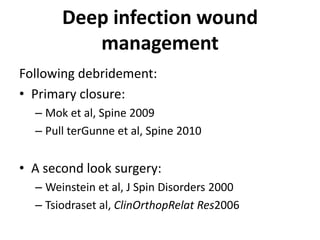
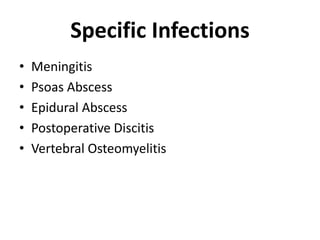
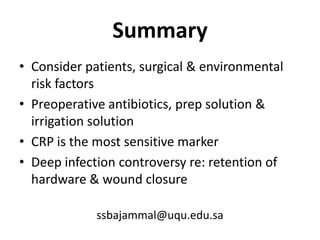
The document discusses the incidence, risk factors, prevention, diagnosis, and treatment of postoperative spinal infections. It emphasizes the importance of preoperative antibiotics and proper surgical techniques to minimize infection rates, as well as the necessity for careful diagnosis and treatment strategies based on infection severity. The findings are based on a systematic review of multiple studies, highlighting the complexity of managing these infections in spinal surgery.