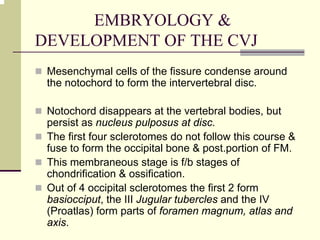
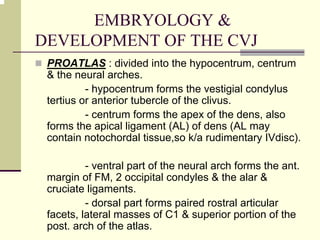
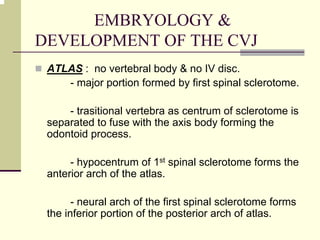
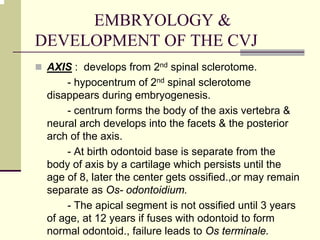
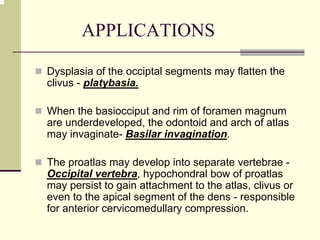
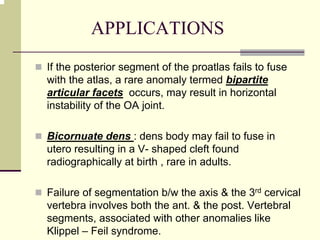
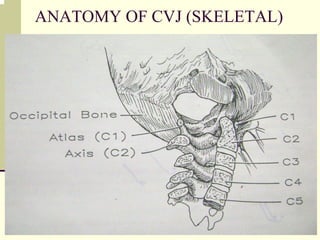
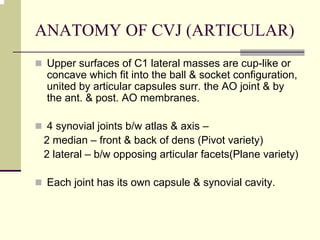
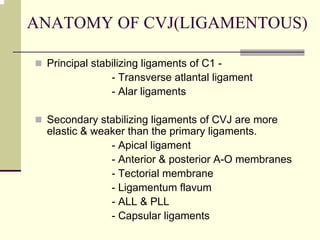
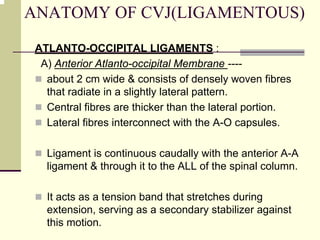
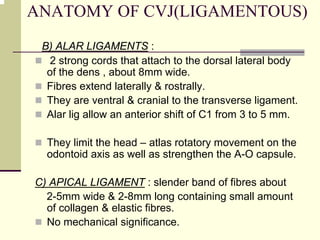
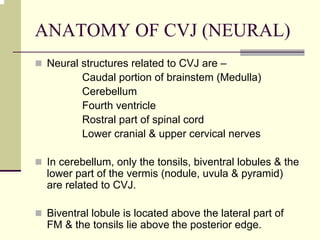
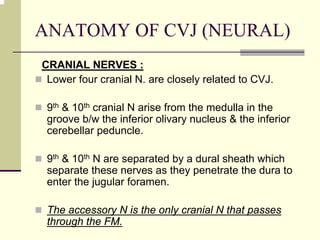
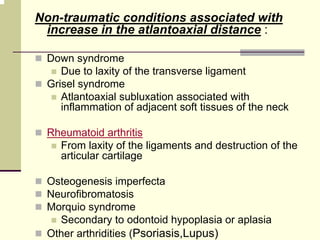
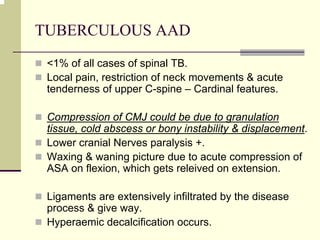
The craniovertebral junction (CVJ) refers to the occiput, atlas, axis, and supporting ligaments. It develops from the occipital somites and proatlas in utero. Key ligaments stabilizing the CVJ include the transverse atlantal ligament, alar ligaments, and apical ligament. Neural structures like the medulla, lower cranial nerves, and vertebral artery pass through the CVJ.