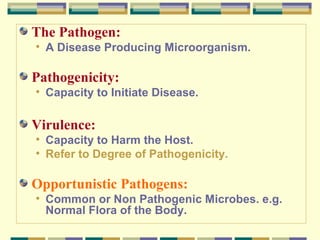
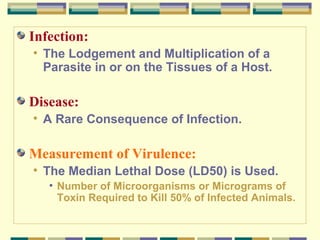
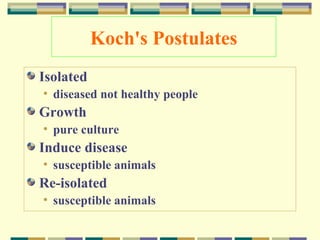
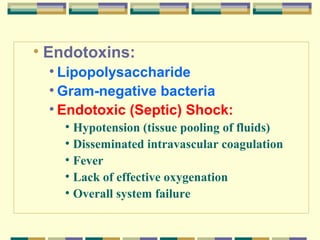
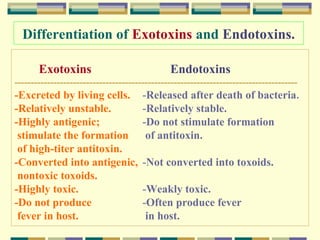
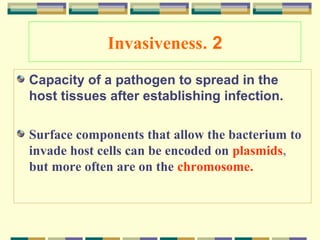
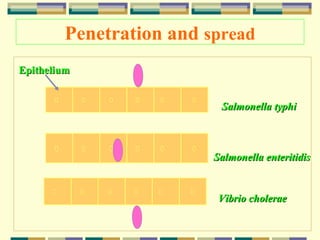
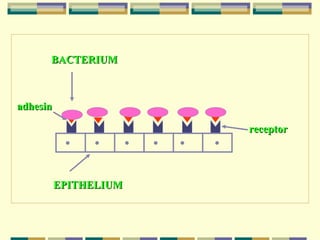
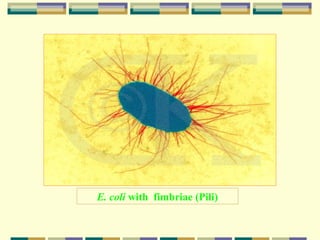
This document provides information on bacterial pathogenesis and virulence factors. It begins with definitions of key terms like pathogens, pathogenicity, virulence, and opportunistic pathogens. It then discusses the difference between infection and disease. Koch's postulates for establishing causation are outlined. The document explores factors that influence pathogenicity like virulence factors, number of initial organisms, and immune status of the host. Several virulence factors are described in detail, including toxins, invasiveness through adhesion and penetration of tissues, capsules that aid evading phagocytosis, siderophores for competing with the host for iron, and enzymes that can aid spreading or hydrolyze immunoglobulins.