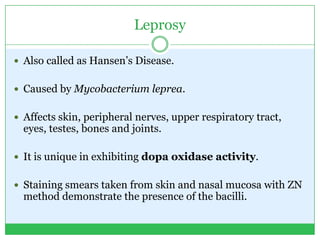
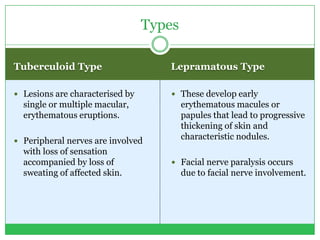
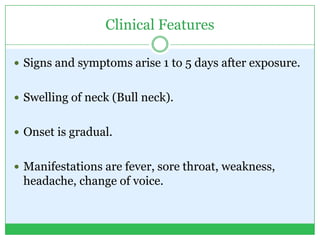
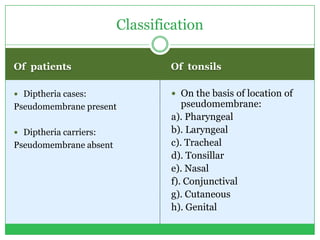
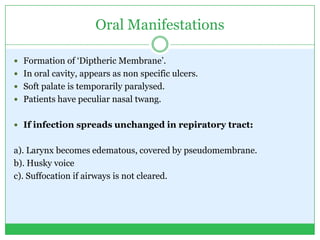
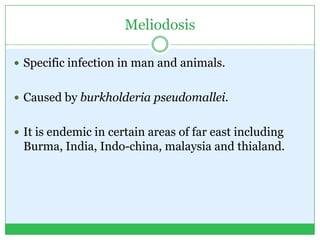
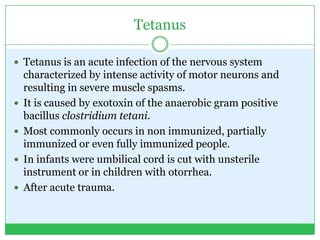
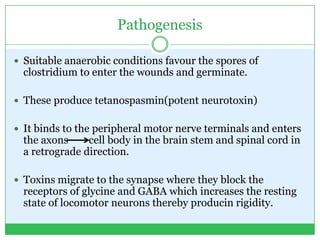
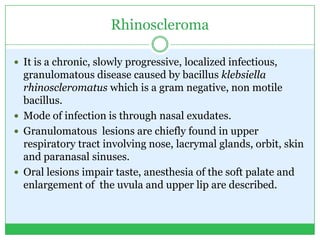
Bacterial infection is caused by disease-causing bacteria invading body tissues. This leads to bacteria multiplying and the body reacting to the microorganisms and toxins they produce. The document discusses many specific types of bacterial infections caused by different bacteria that affect various parts of the body, including their symptoms, pathogenesis, diagnosis and treatment.