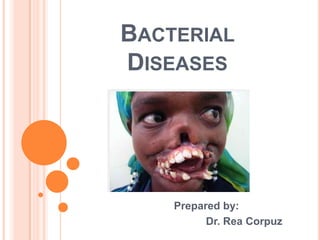
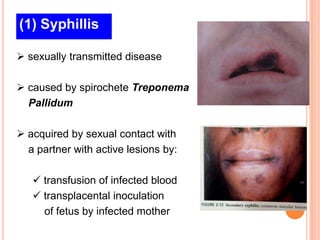
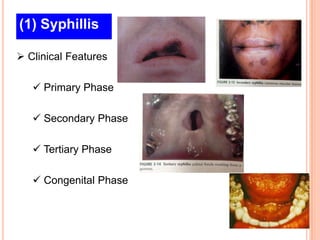
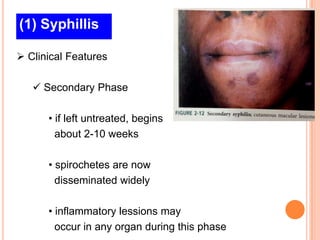
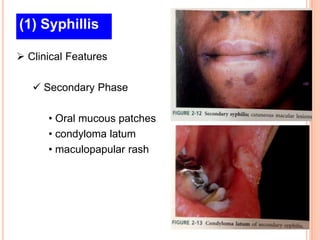
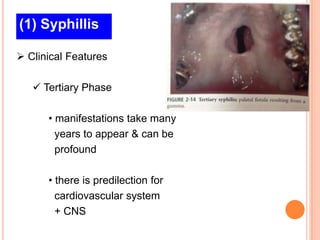
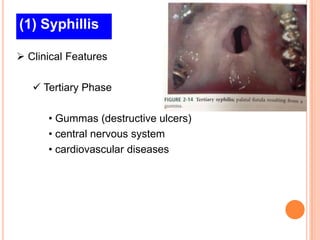
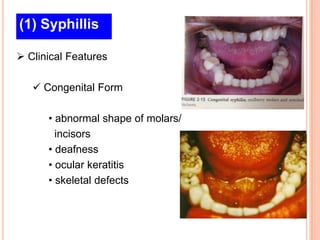
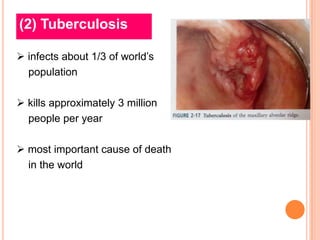
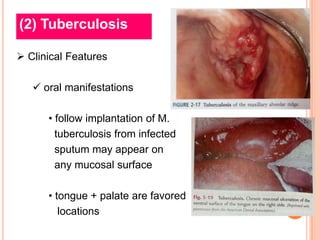
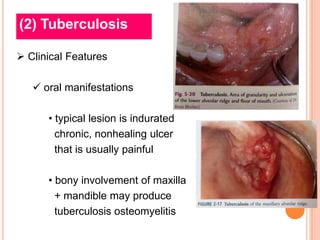
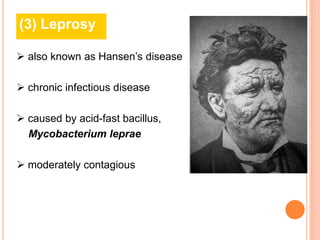
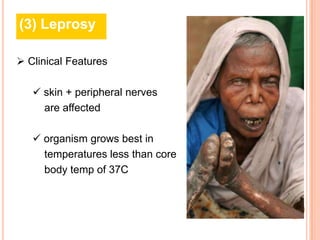
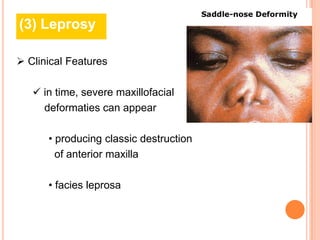
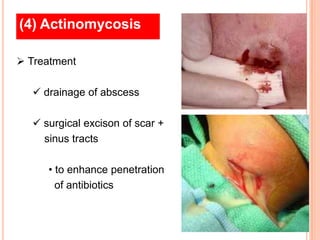
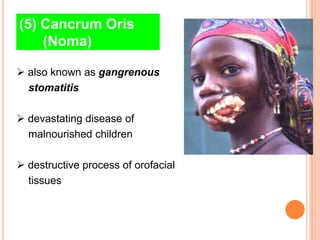
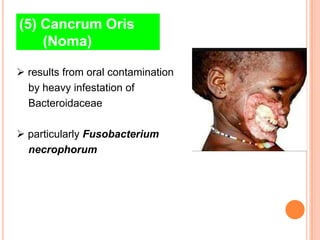
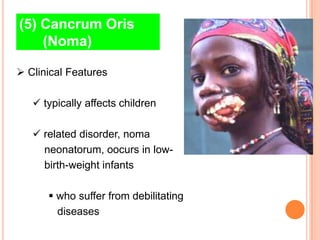
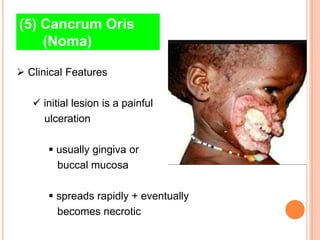
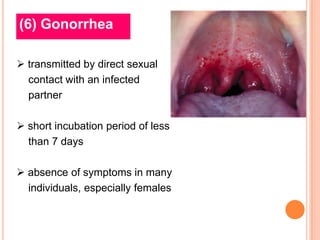
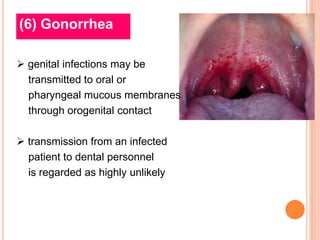
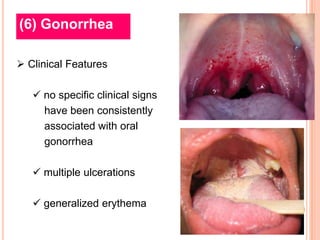
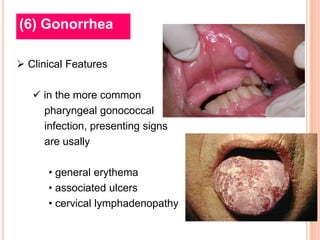
The document discusses 6 bacterial diseases: syphilis, tuberculosis, leprosy, actinomycosis, cancrum oris (noma), and gonorrhea. It provides details on the causative bacteria, pathogenesis, clinical features, and treatment for each disease. Syphilis is caused by Treponema pallidum and has primary, secondary, tertiary, and congenital stages. Tuberculosis is caused by Mycobacterium tuberculosis and can cause oral lesions. Leprosy is caused by Mycobacterium leprae and has a spectrum of manifestations. Actinomycosis is caused by Actinomyces israelii and usually follows trauma. Cancrum oris