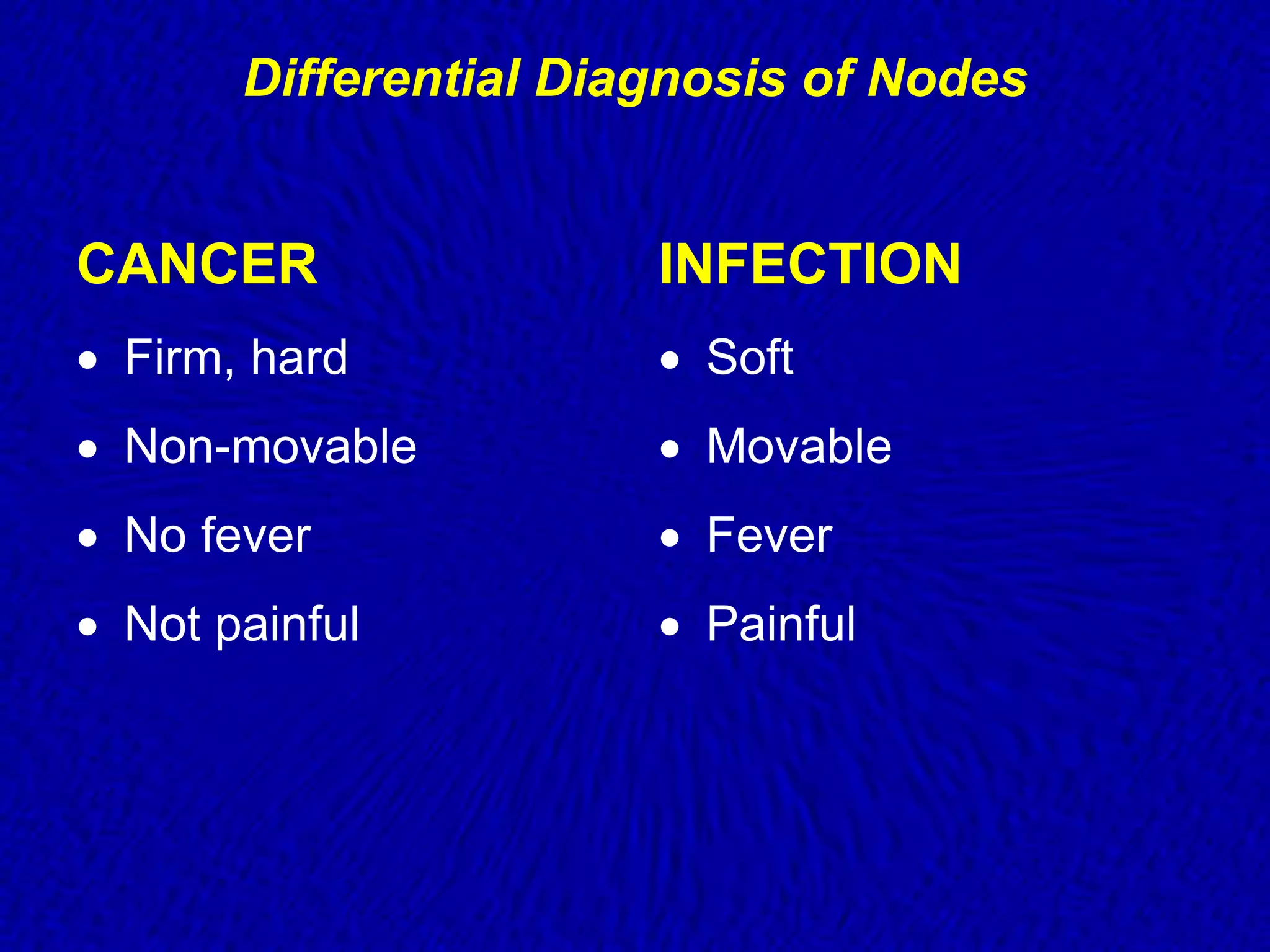
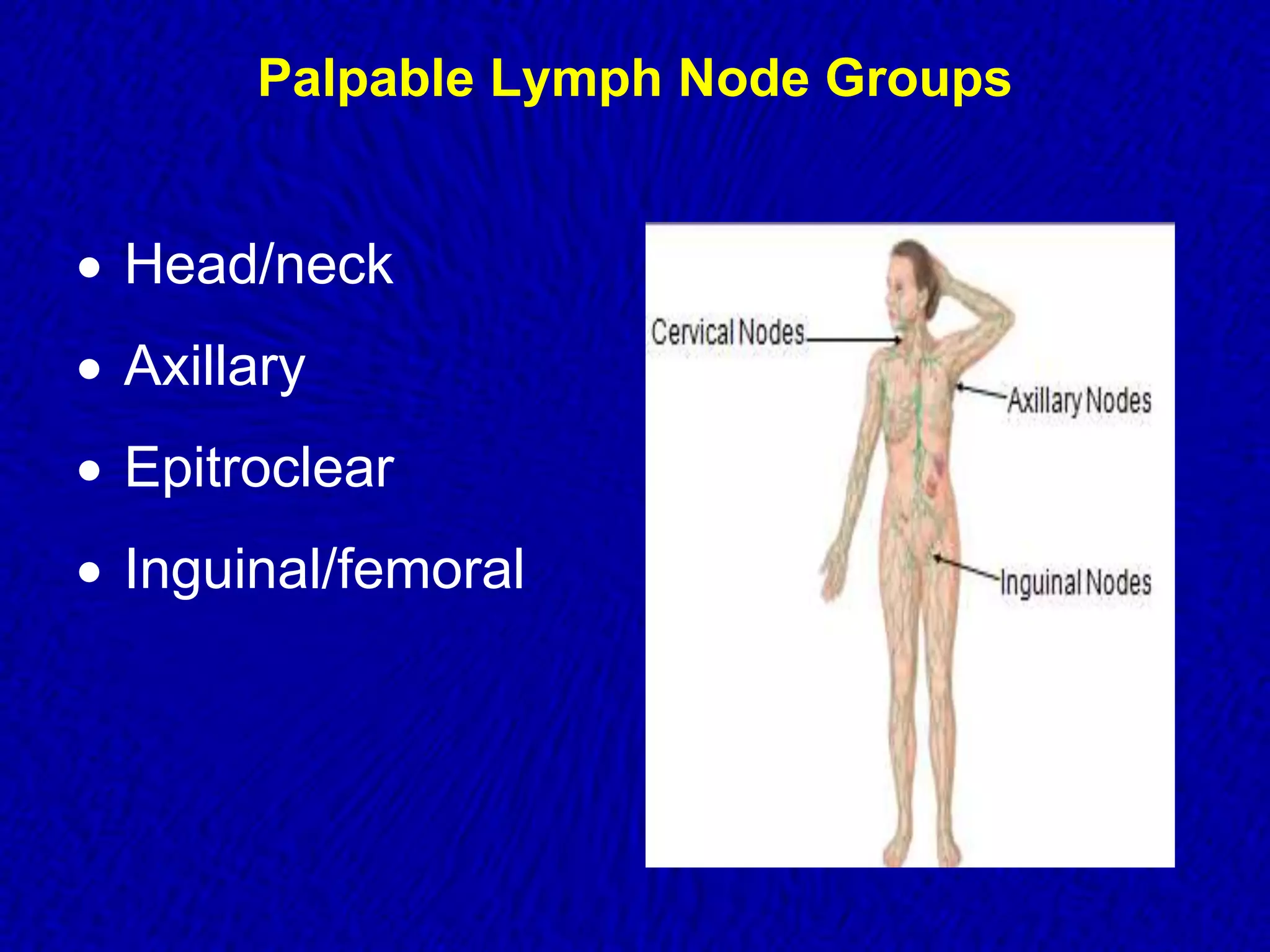
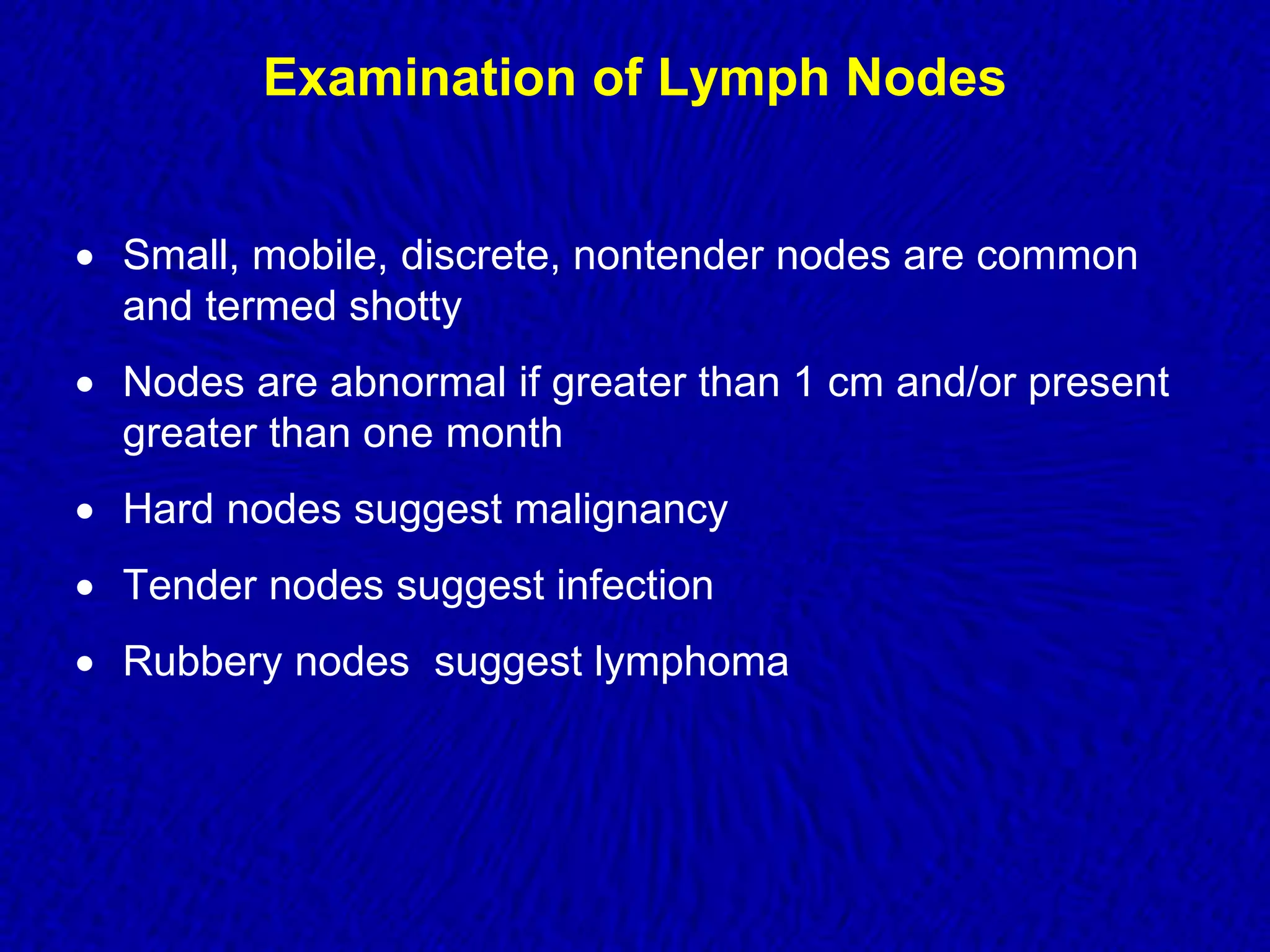
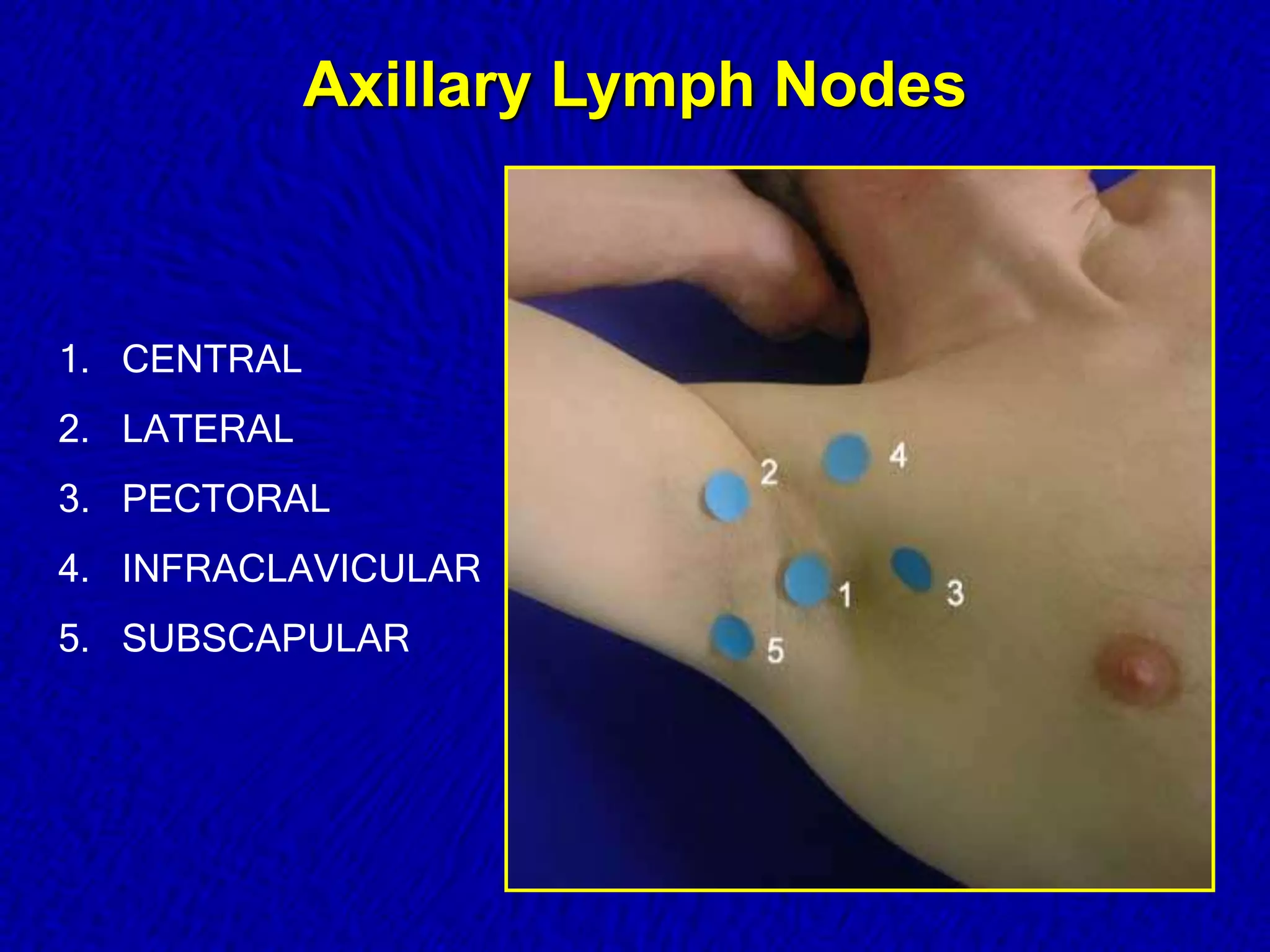
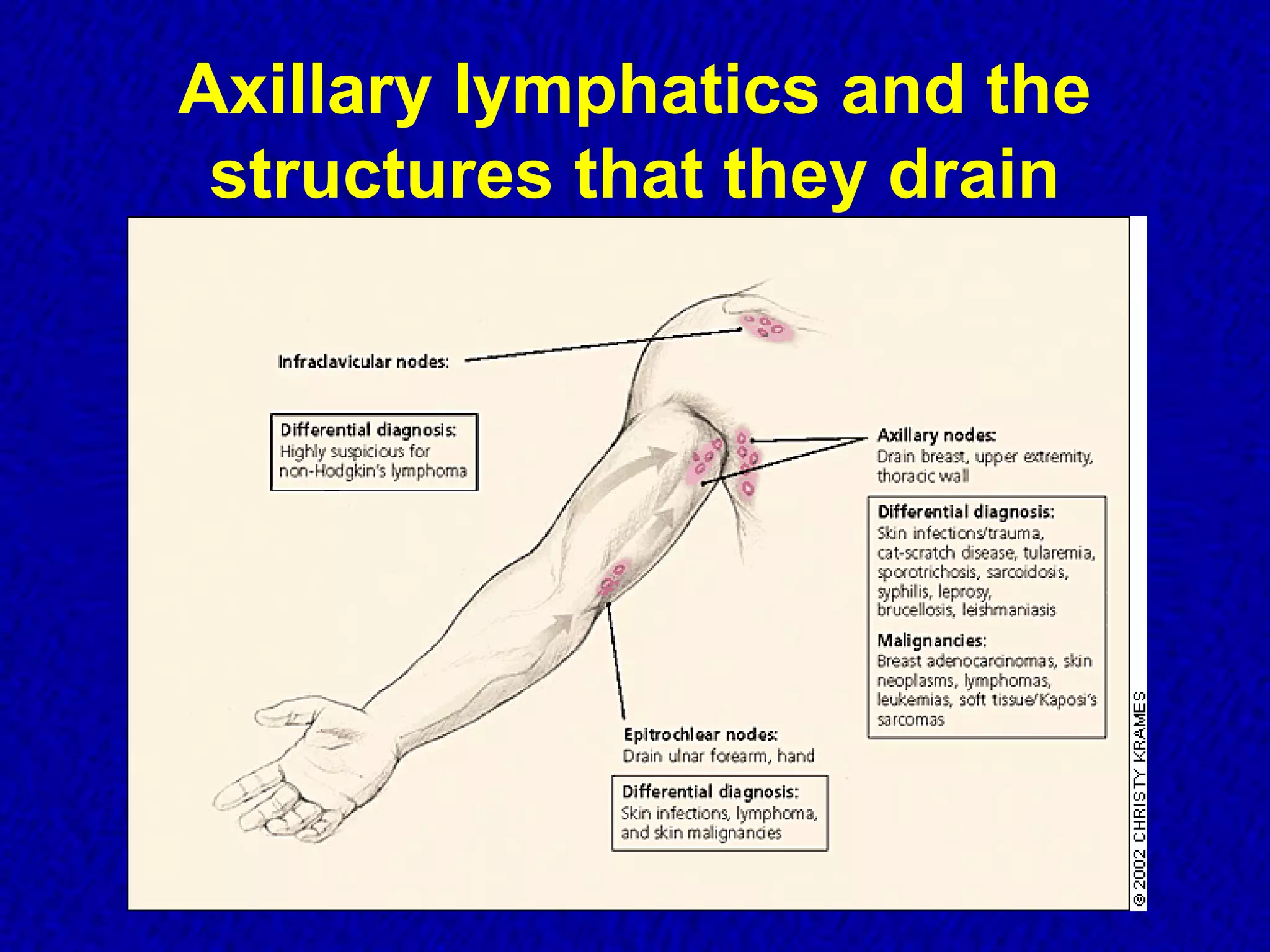
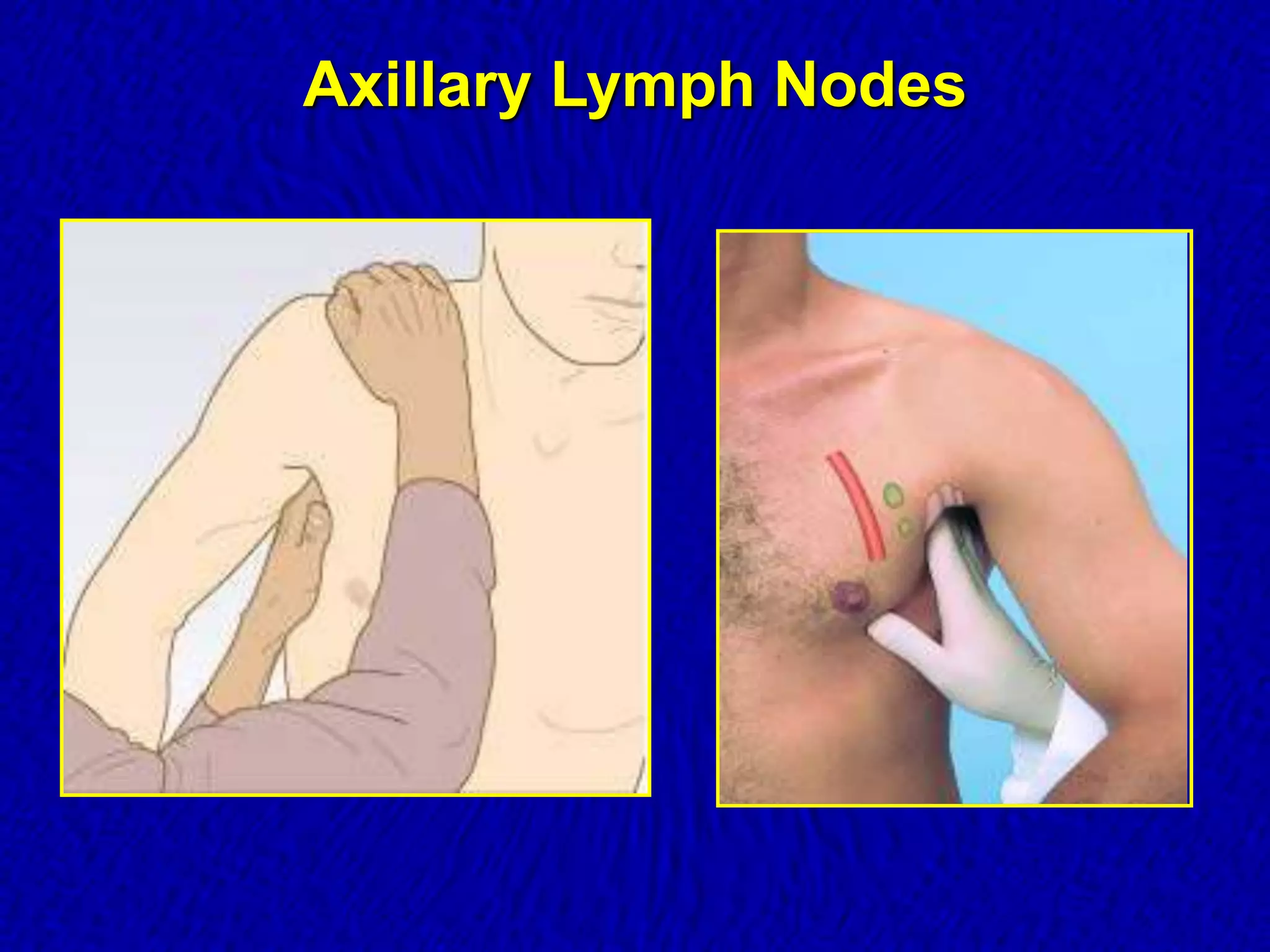
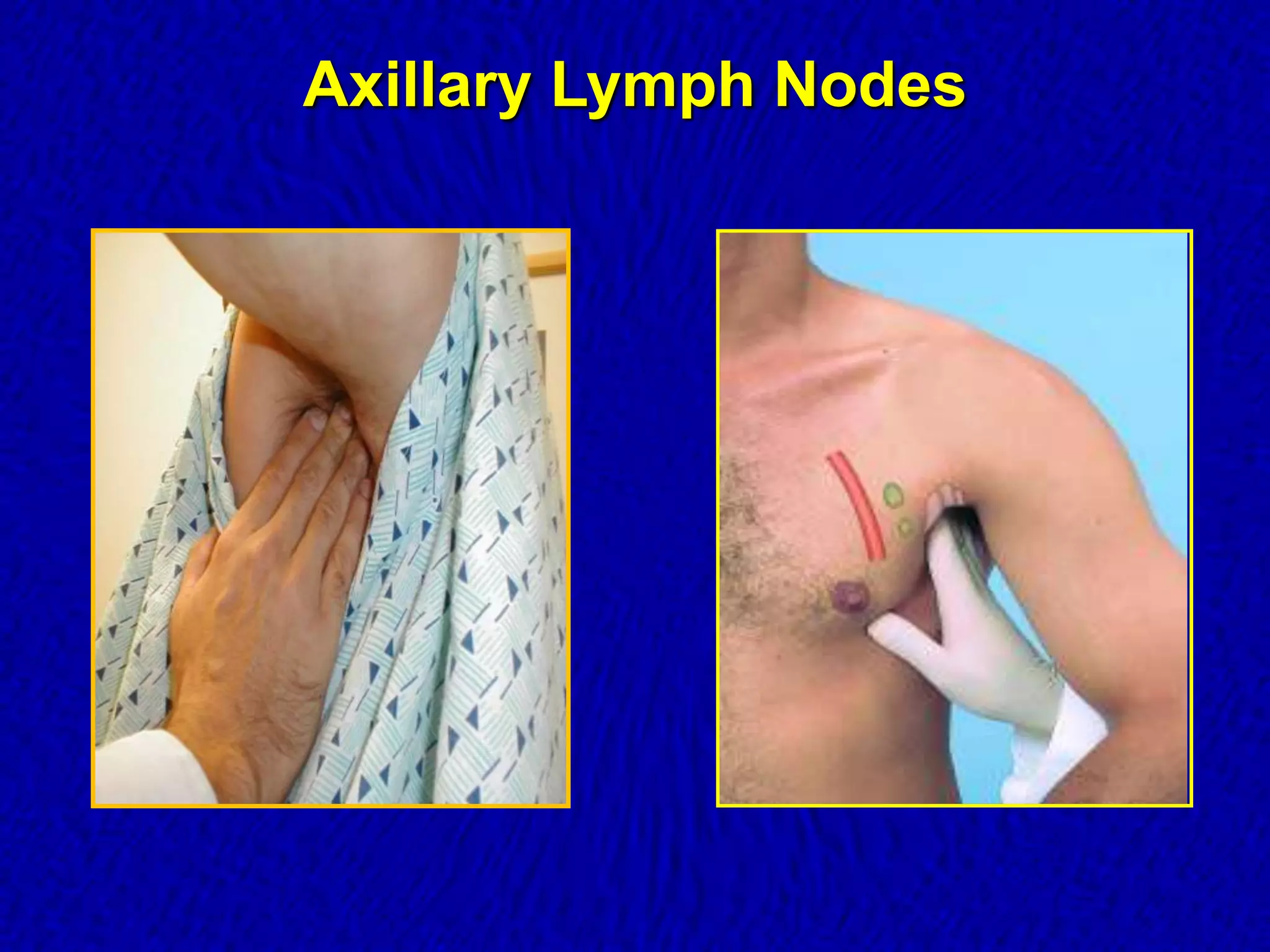
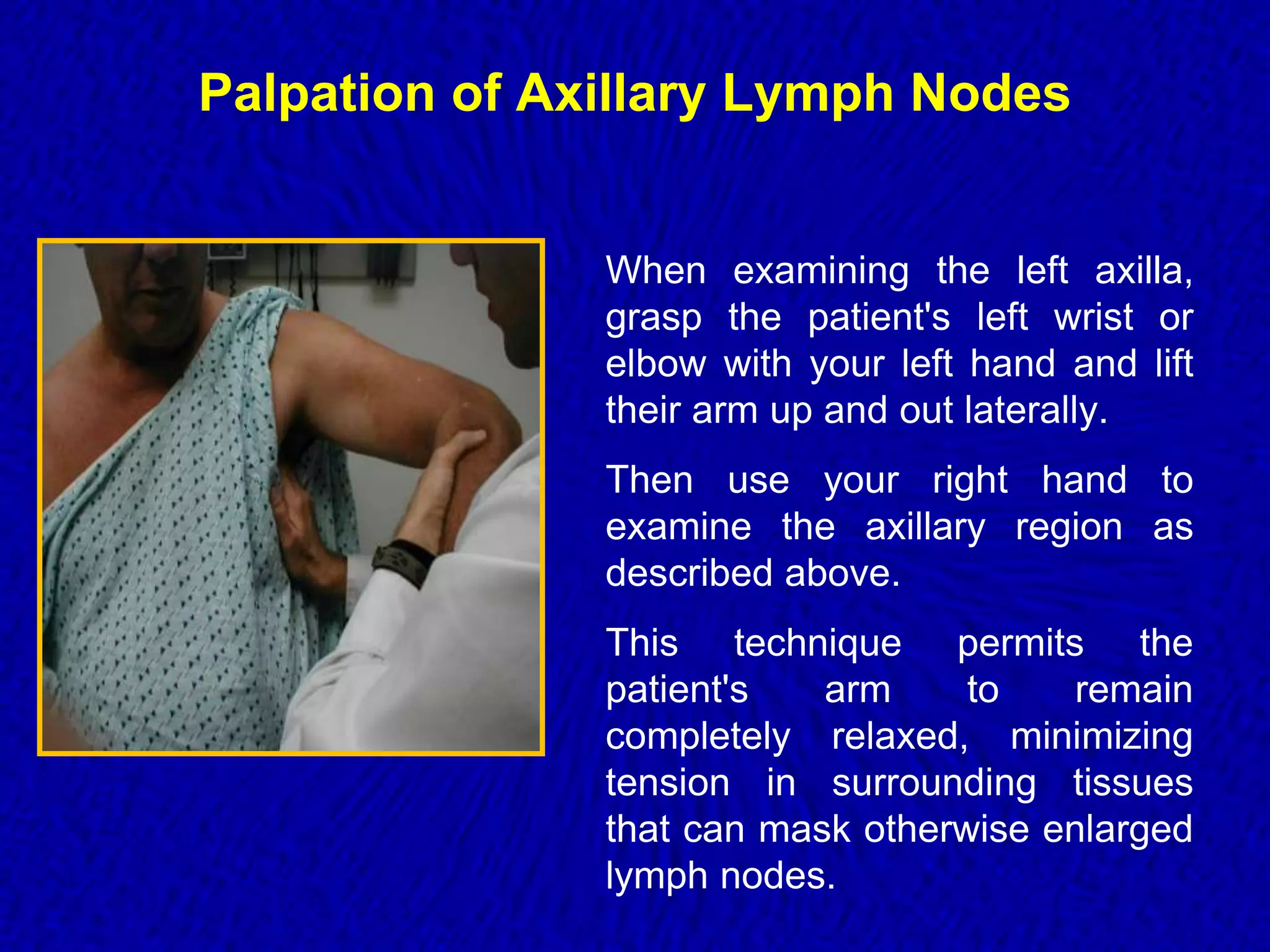
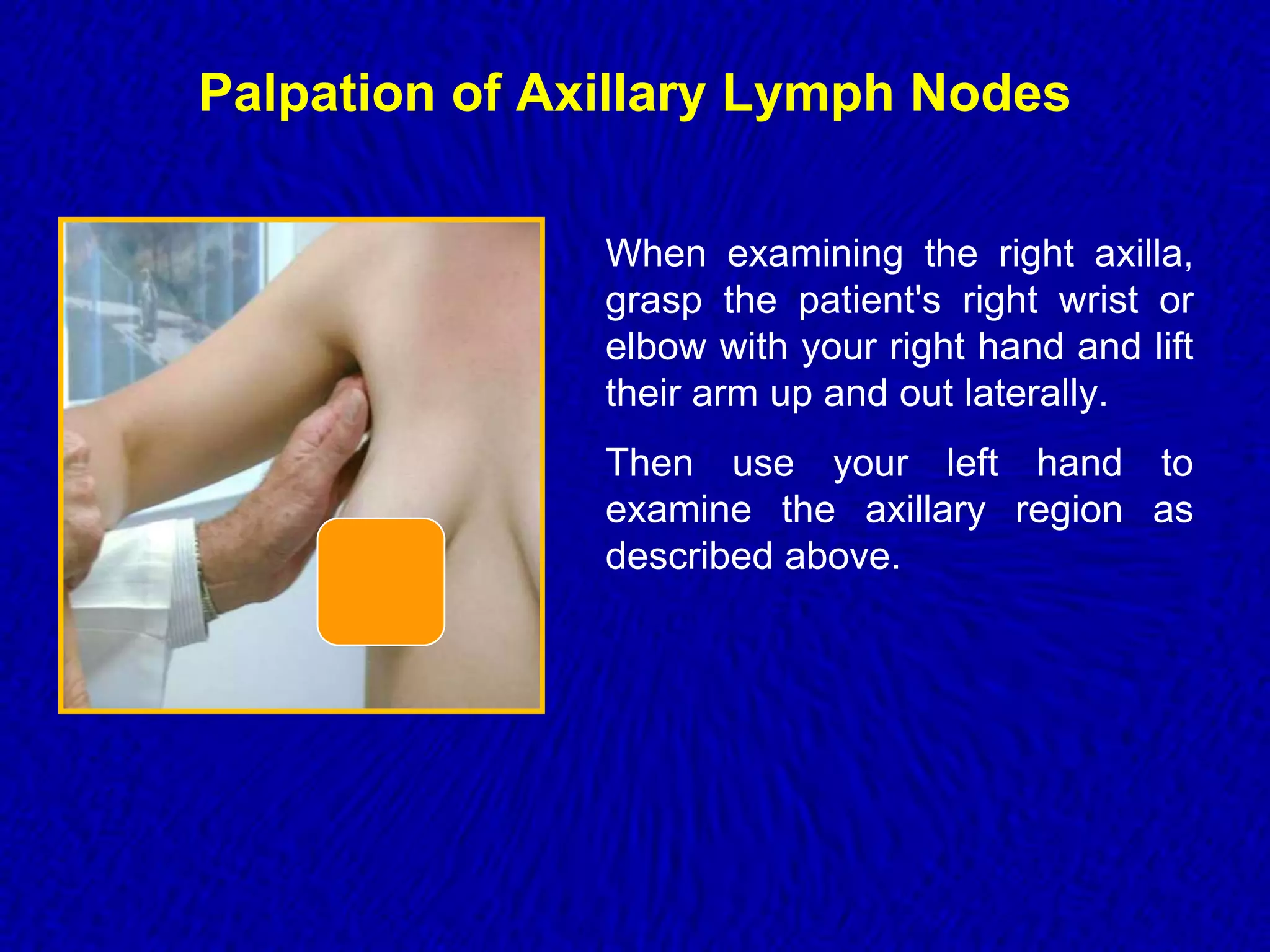
This document discusses examination of the axillary lymph nodes. It describes how to inspect and palpate the axillary region to examine the lymph nodes located there. Specific lymph node groups in the axilla are identified. Enlarged or abnormal lymph nodes may suggest issues like infection or cancer that require further examination of the primary site and other lymph node areas. The size, texture, tenderness and mobility of lymph nodes can provide clues to potential diagnoses.