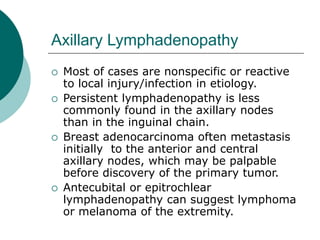
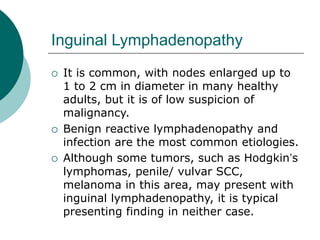
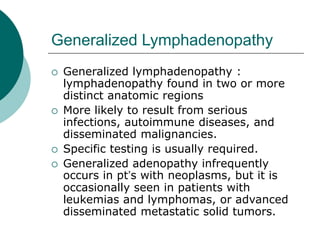
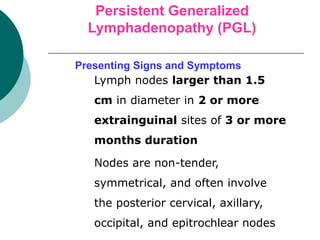
Lymphadenopathy can be caused by malignancies, infections, autoimmune disorders, or other miscellaneous conditions. Evaluation involves considering the patient's age, duration of lymphadenopathy, exposures, associated symptoms, and physical examination findings regarding nodal character and size. For unexplained lymphadenopathy lasting over a month, specific investigation such as biopsy may be needed. Biopsy of the largest, most suspicious node can help arrive at a diagnosis and guide further management. Persistent generalized lymphadenopathy also requires consideration of underlying causes such as HIV.