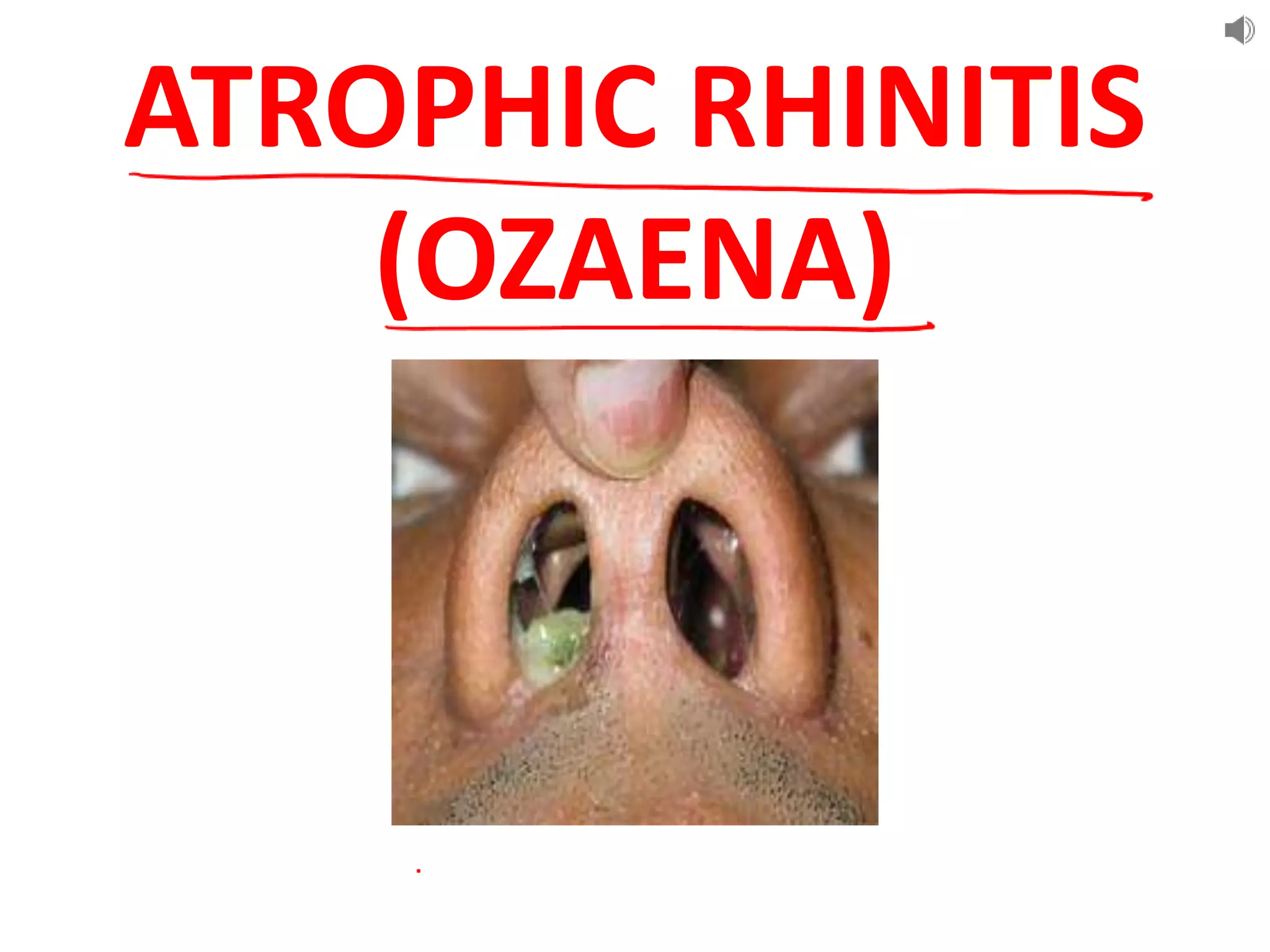
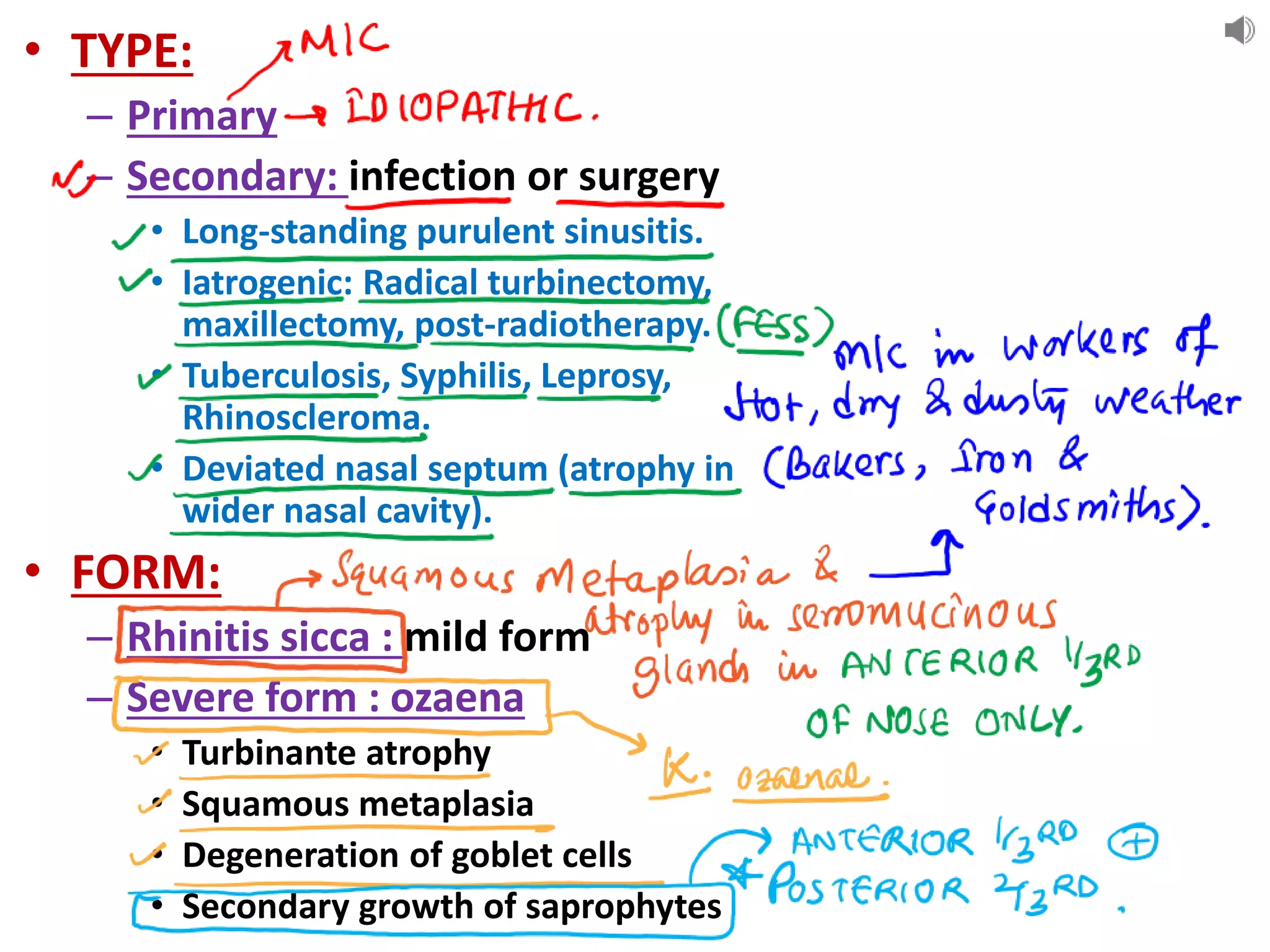
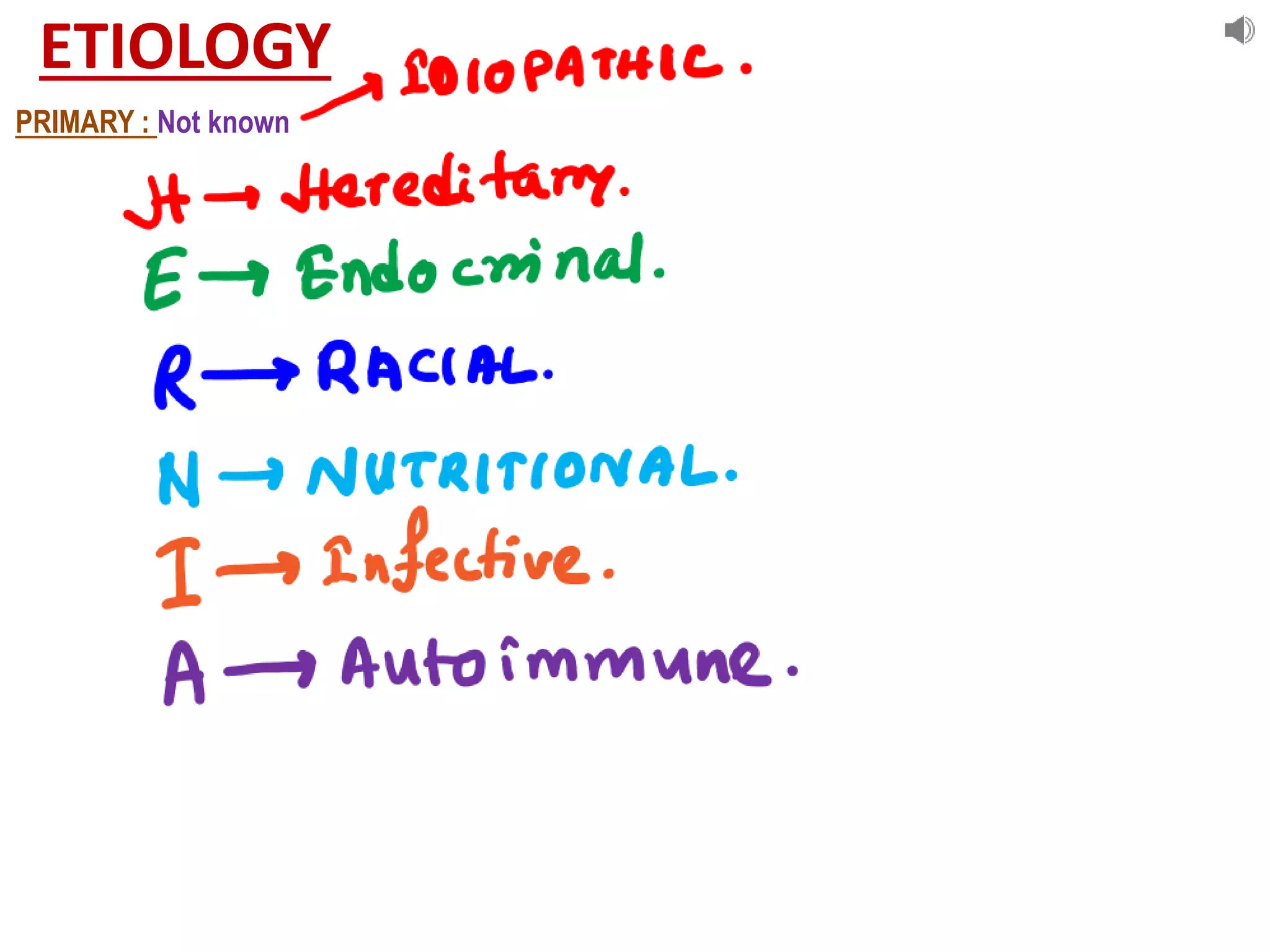
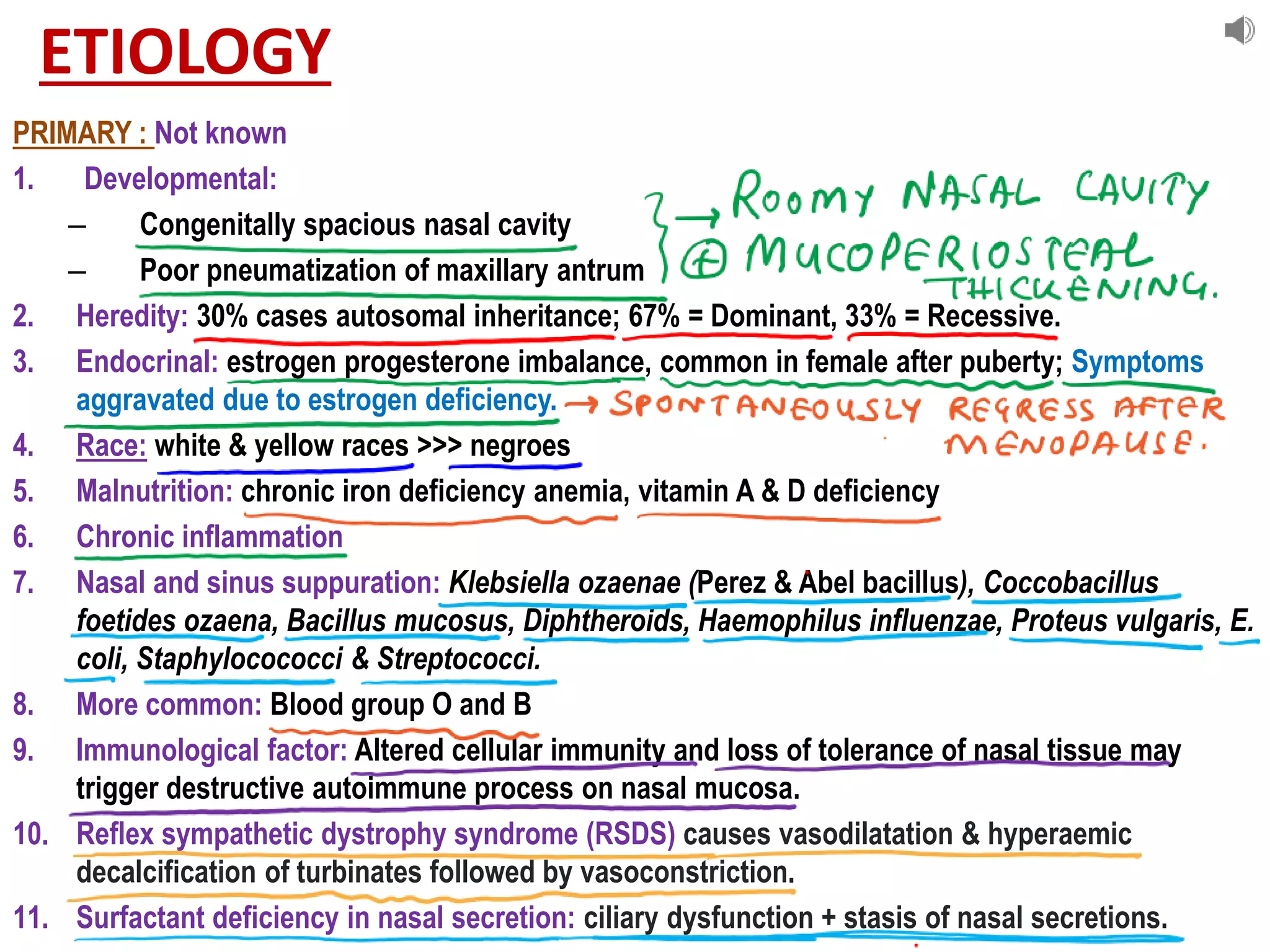
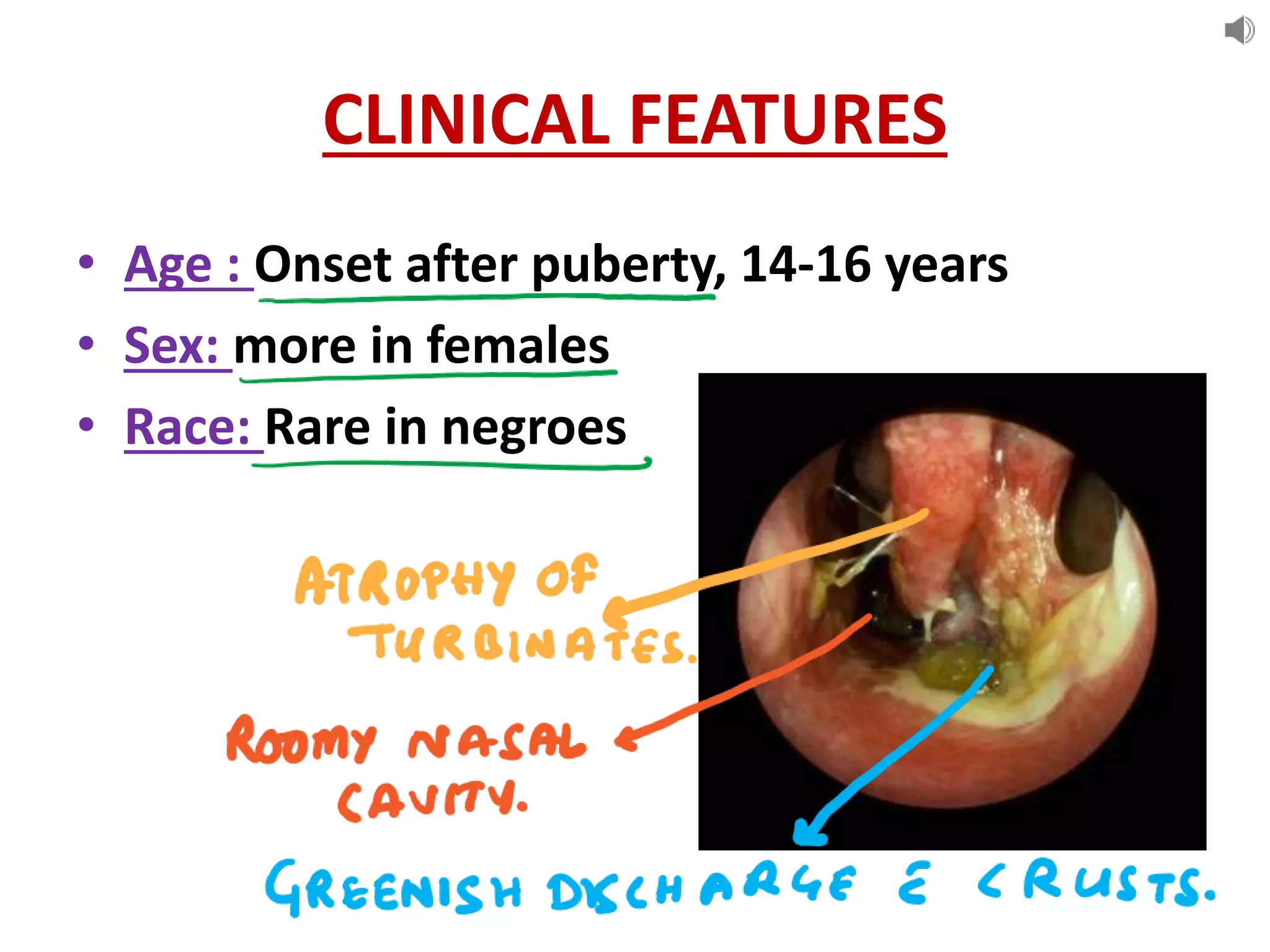
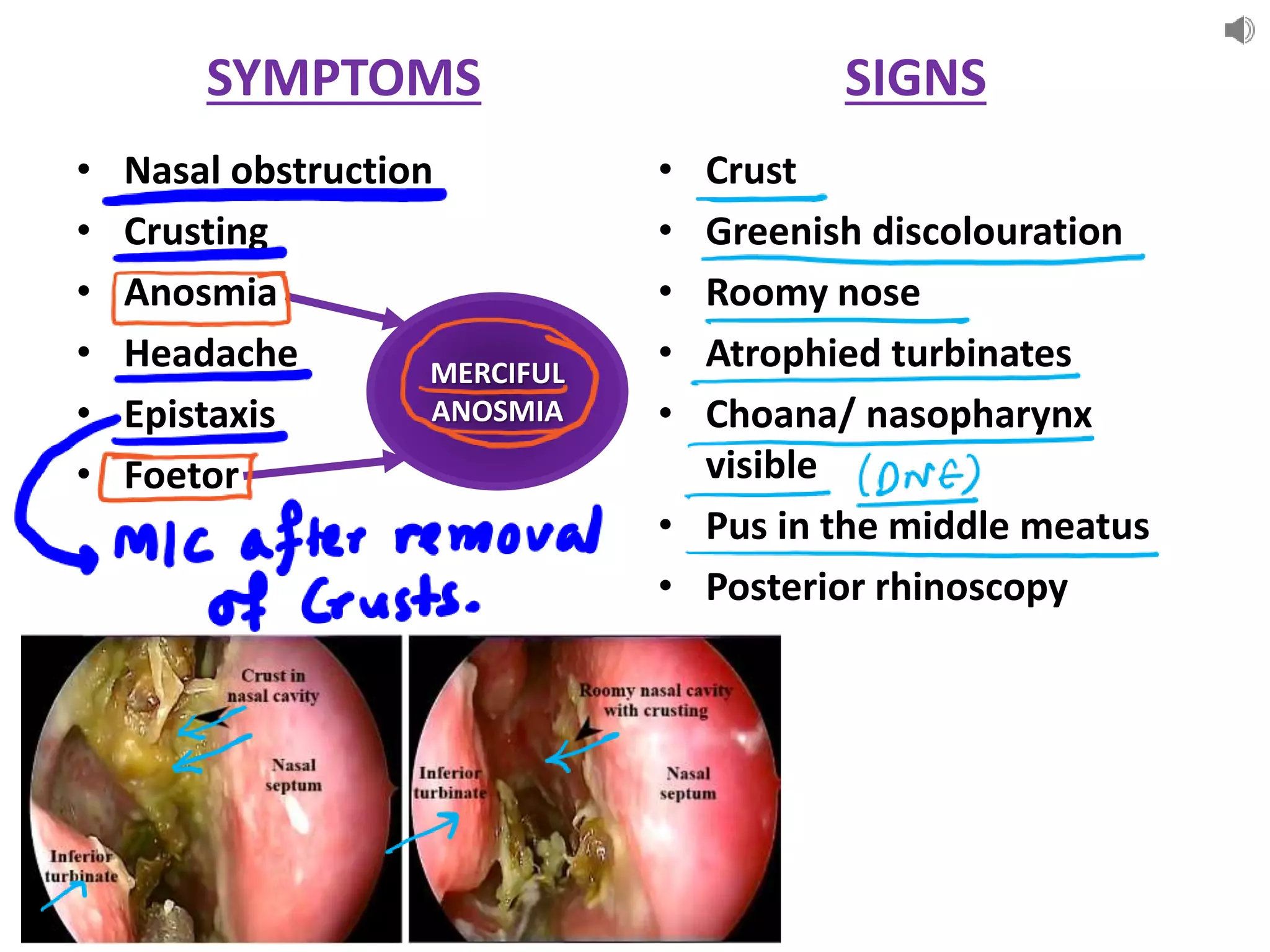
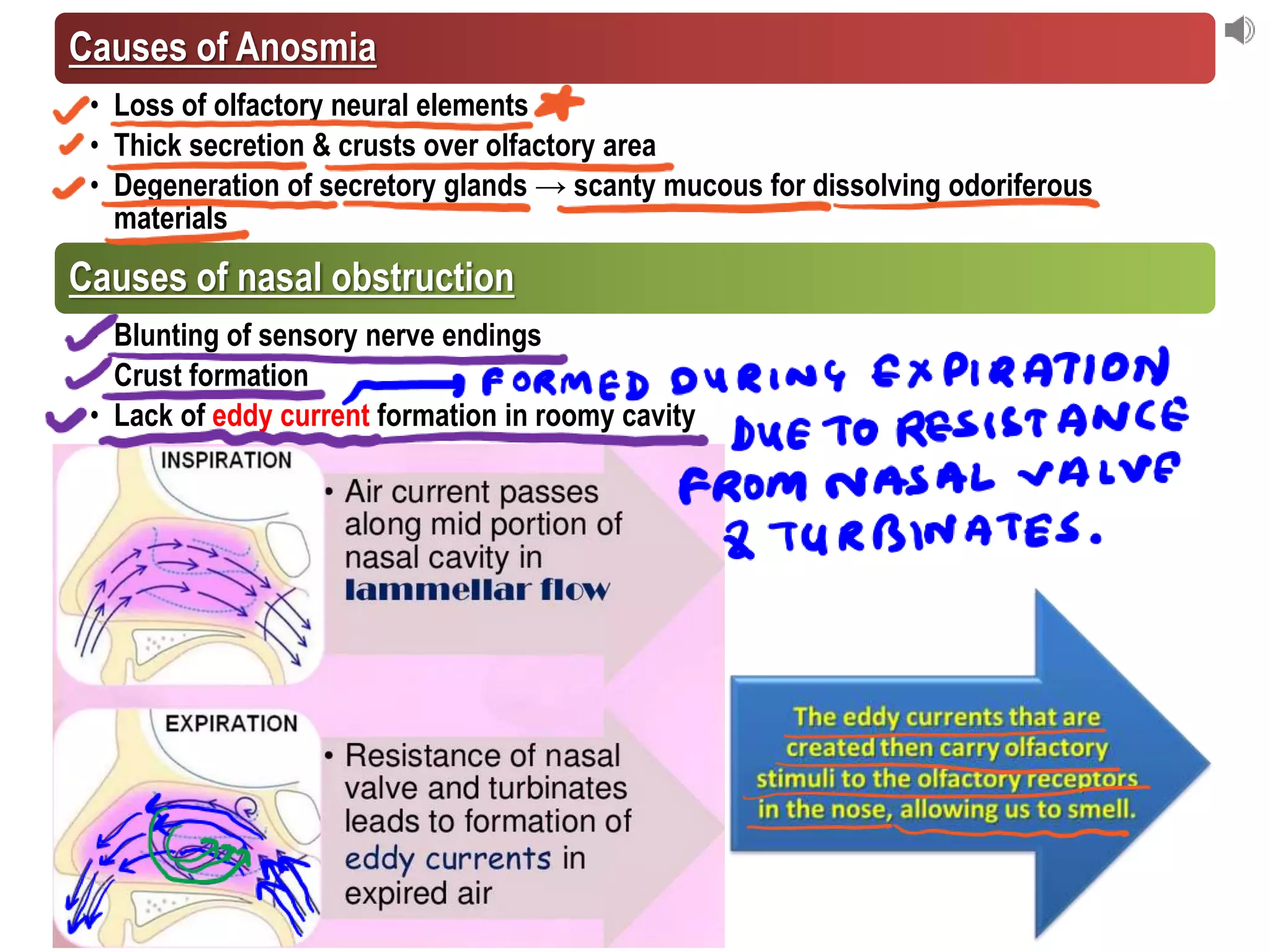
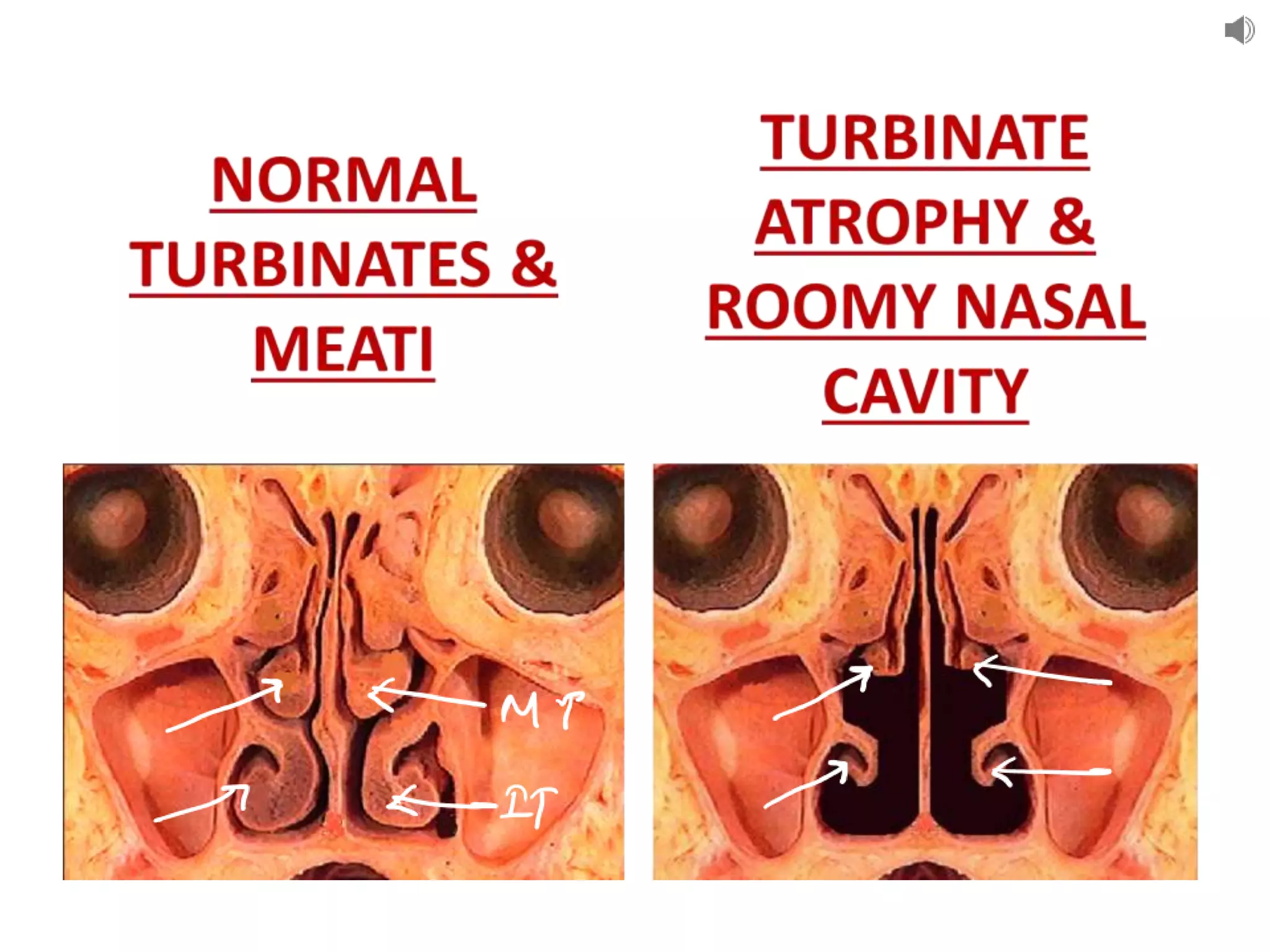
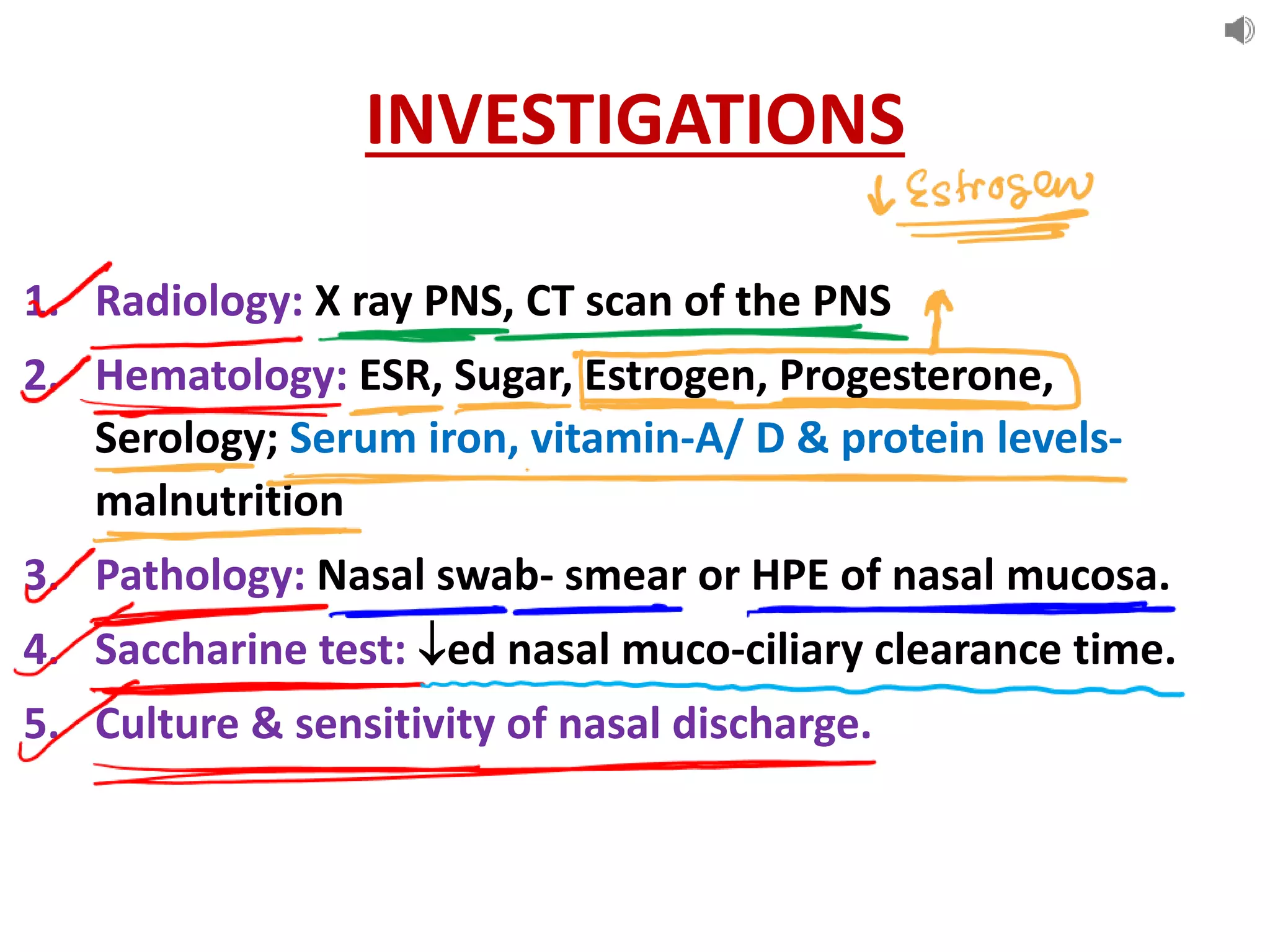
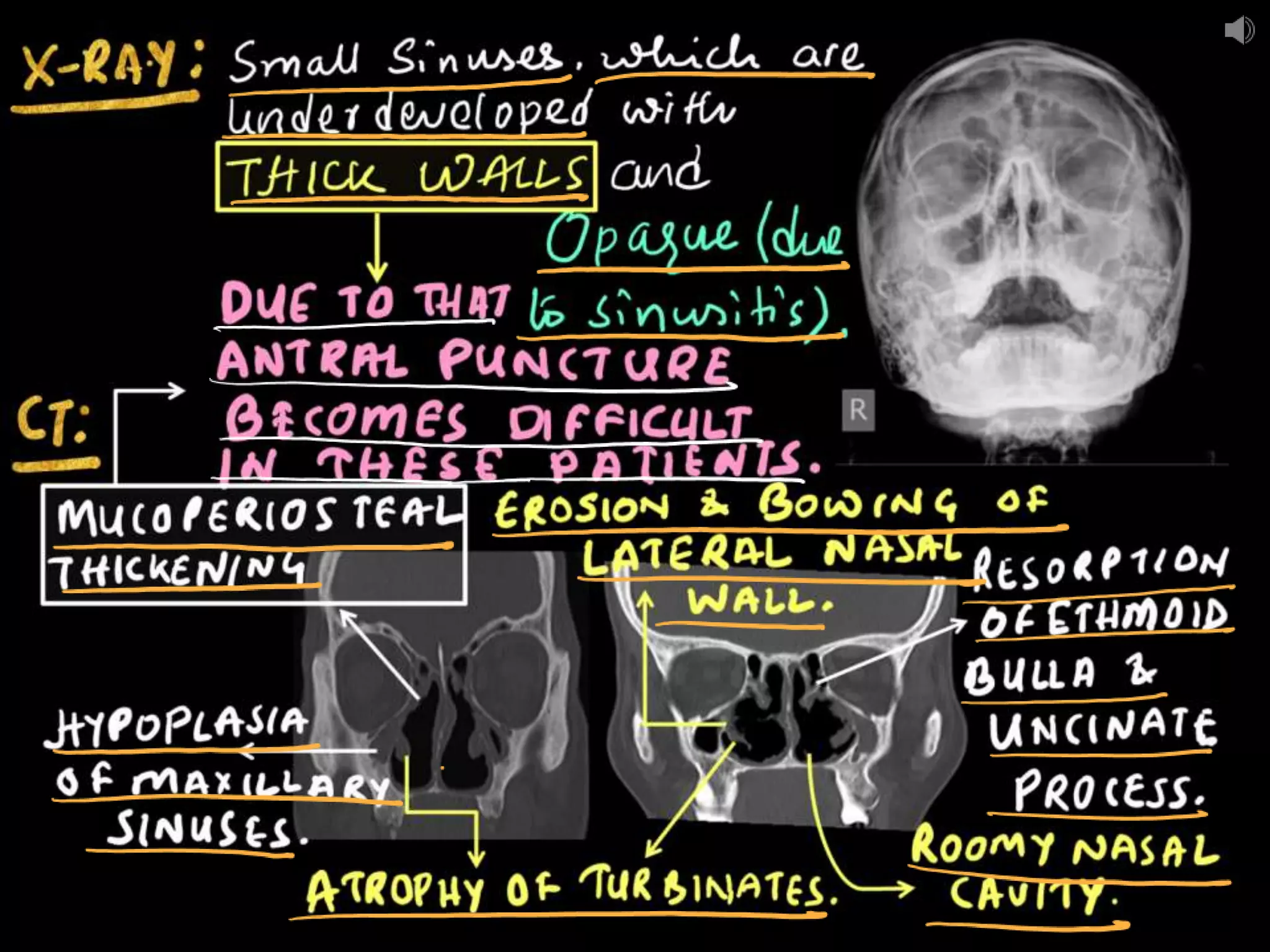
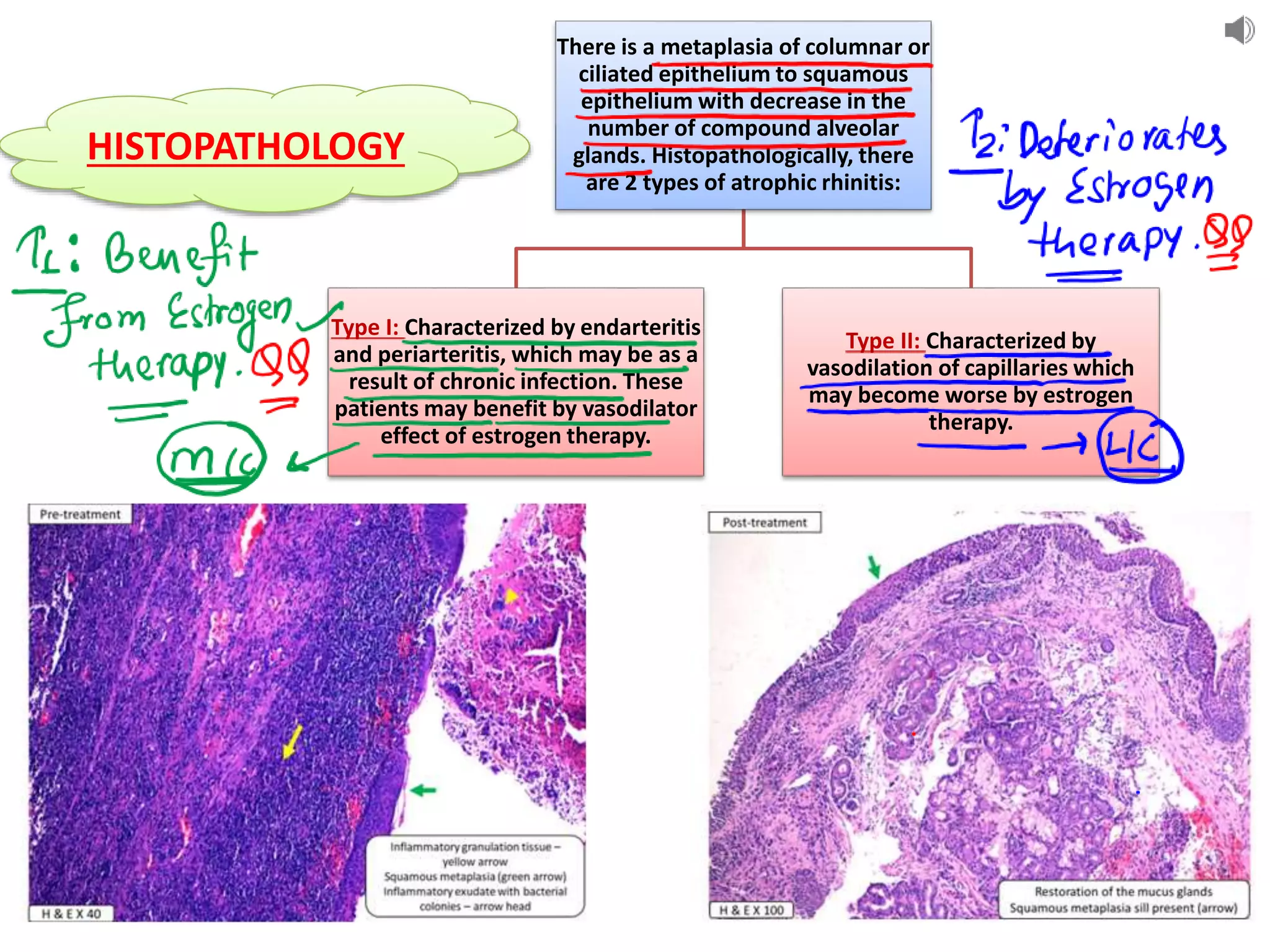
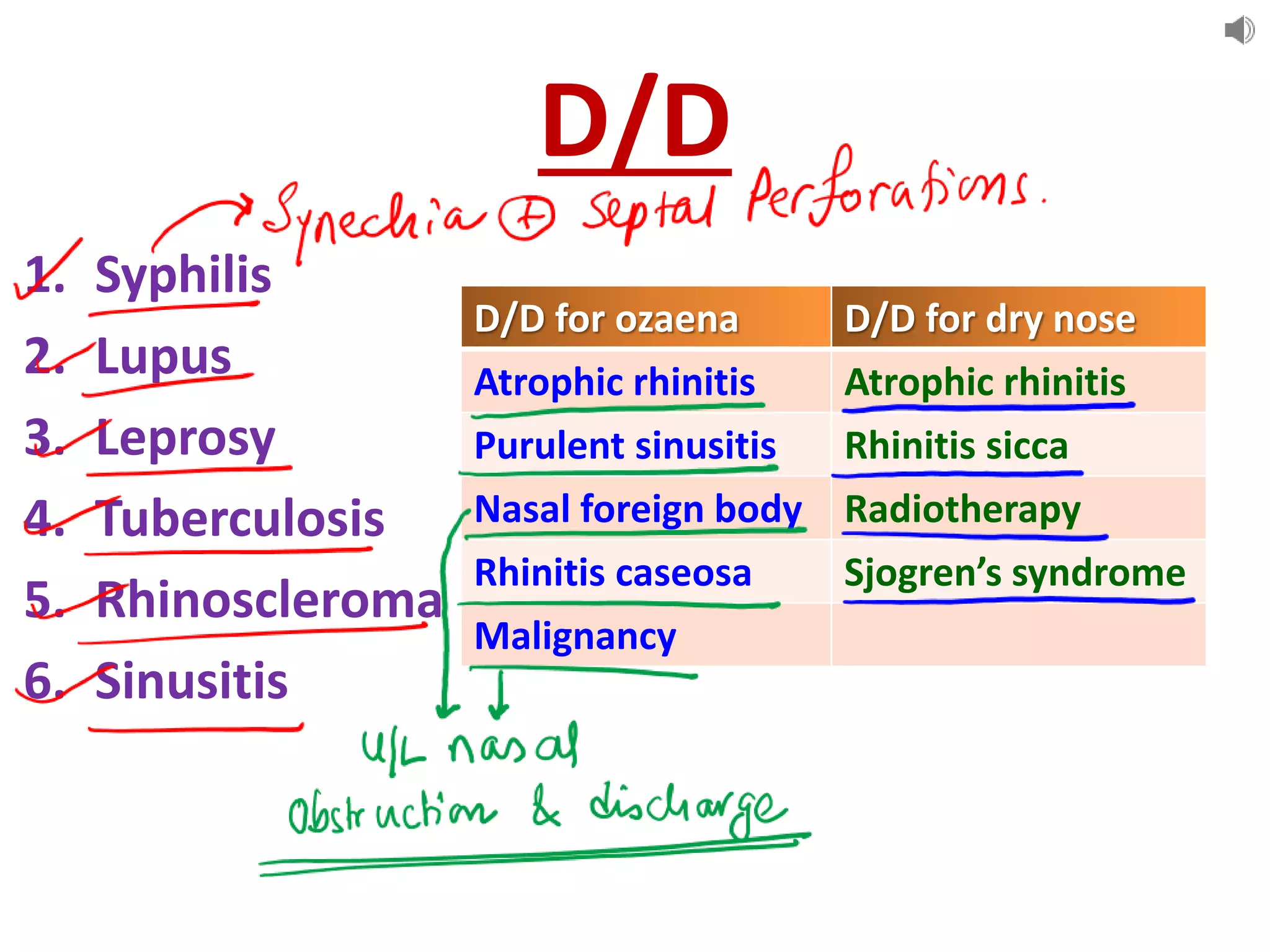
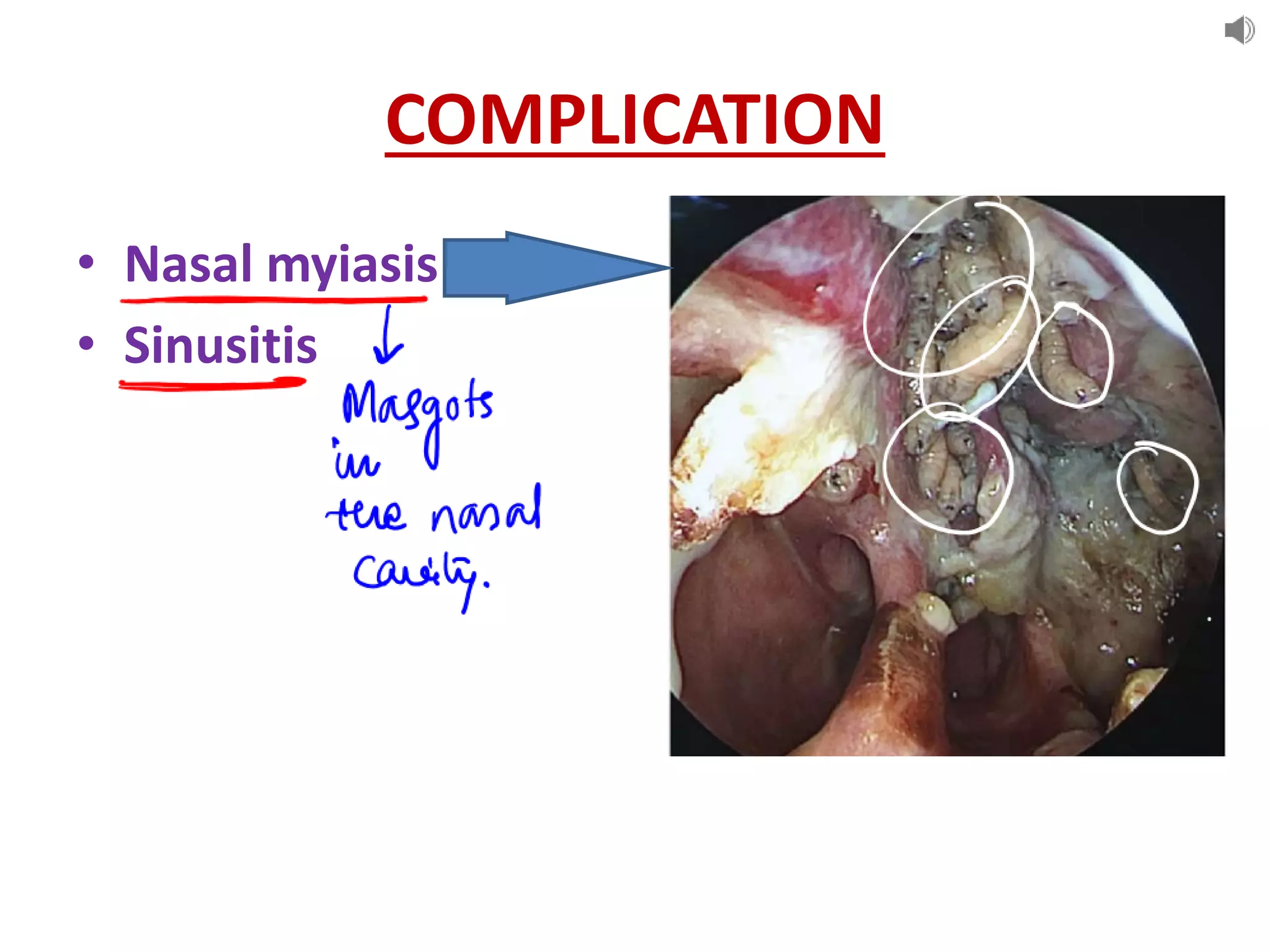
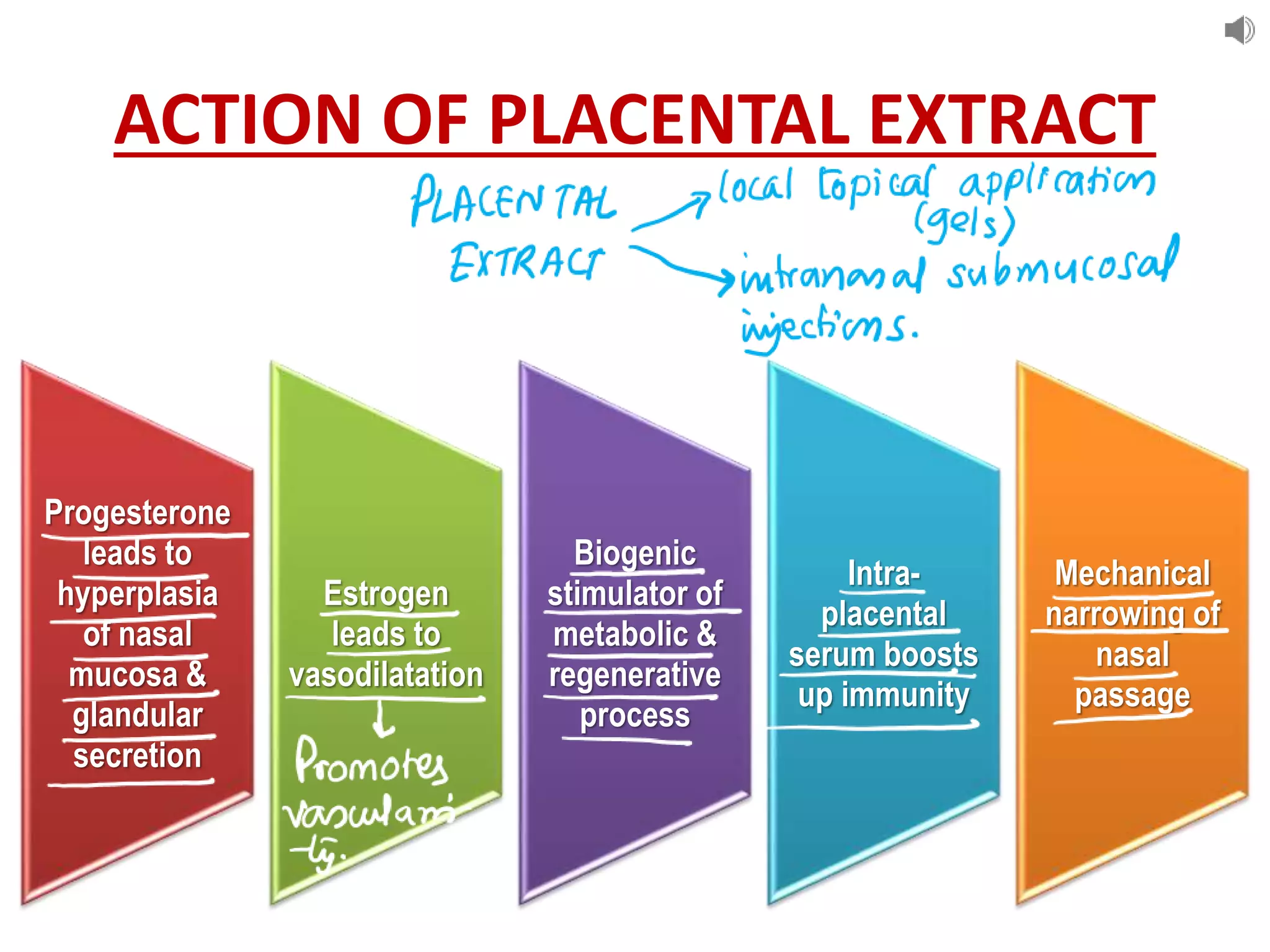
Atrophic rhinitis, also known as ozaena, is a chronic inflammation of the nasal mucosa that results in atrophy, squamous metaplasia, and crust formation. It is characterized by the atrophy of the nasal mucosa and turbinates, scanty viscid secretions, loss of ciliated columnar epithelium, and crust formation. The pathophysiology involves periarteritis and endarteritis of the nasal mucosa, decreasing blood supply and resulting in atrophy of mucous glands, epithelium, and metaplasia of the ciliated columnar epithelium. Treatment involves antibiotics, estrogen therapy, surgical procedures to narrow the nasal cavity and increase lubrication, and sal