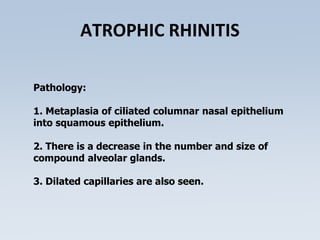
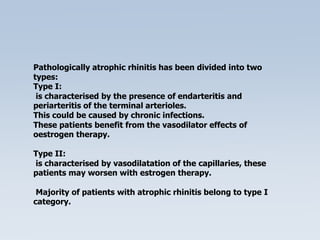
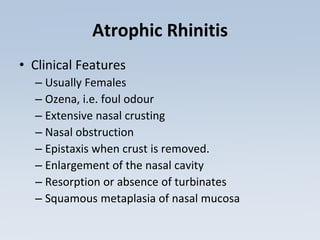
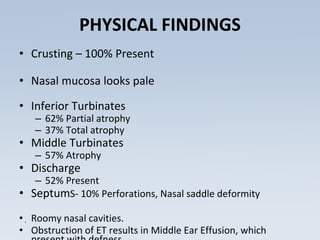
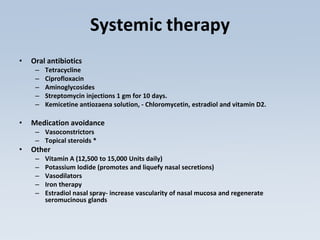
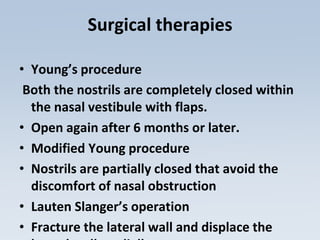
Atrophic rhinitis is a chronic nasal disease characterized by progressive atrophy of the nasal mucosa and underlying bone of the turbinates. It causes foul-smelling crusts to form from thick secretions. The cause is unclear but may involve nutritional deficiencies or chronic infections by organisms like Klebsiella ozaenae. Clinically, patients experience nasal obstruction and crusting with an unpleasant odor. Treatment focuses on irrigation to restore hydration and minimize crusts, along with systemic antibiotics and surgery to reconstruct the nasal cavity.