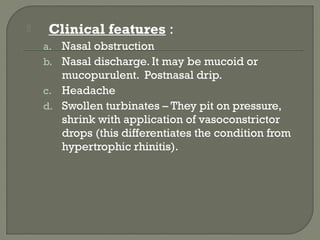
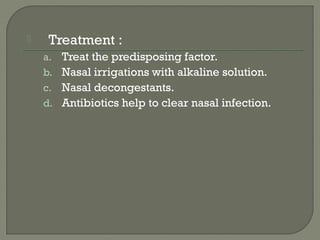
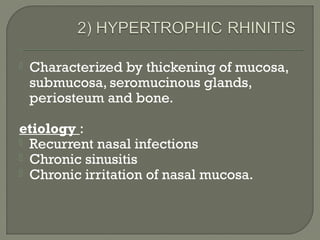
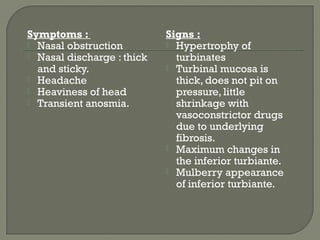
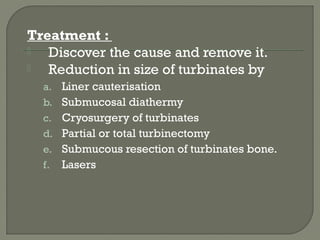
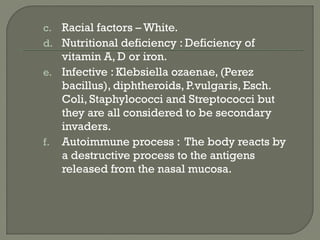
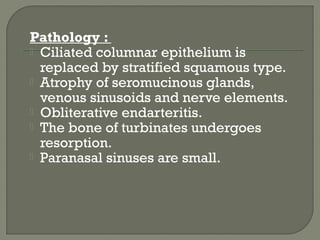
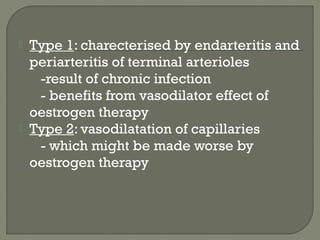
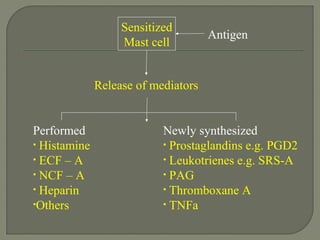
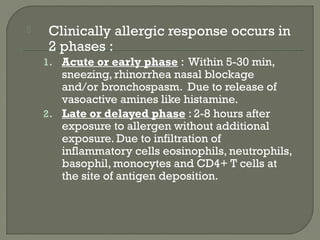
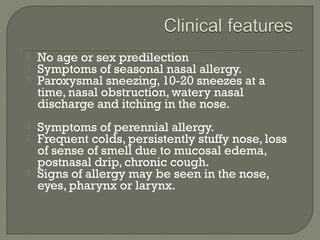
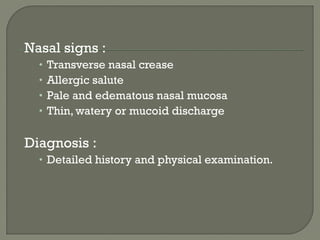
This document summarizes different types of rhinitis including common cold, influenza rhinitis, allergic rhinitis, vasomotor rhinitis, chronic rhinitis, atrophic rhinitis, and hypertrophic rhinitis. It describes the etiology, clinical features, treatment, and complications of each type. The types are distinguished based on their causes such as viruses, allergens, chronic infections, or autonomic imbalances. Treatment involves managing the underlying cause as well as medications to reduce symptoms like antihistamines, decongestants, corticosteroids, and immunotherapy for allergic rhinitis.