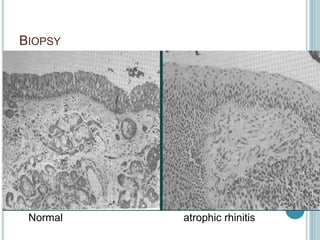
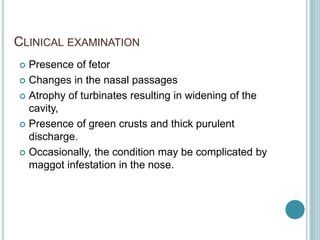
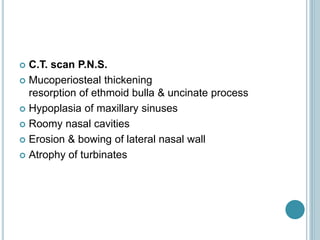
Atrophic rhinitis is a chronic nasal disease characterized by atrophy of the nasal mucosa and bone of the turbinates. It is associated with thick, foul-smelling secretions and crust formation. The cause is often unknown but may be due to infections, surfactant deficiency, or autonomic imbalances. Treatment involves regular nasal cleansing, topical medications to hydrate the nose, systemic antibiotics, and sometimes surgery to decrease nasal volume or improve vascularity.