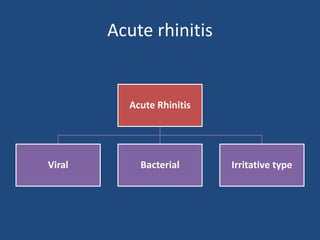
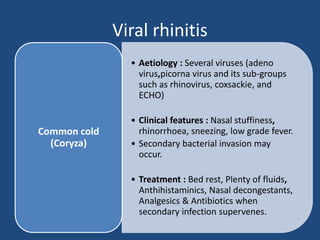
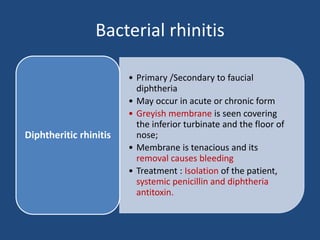
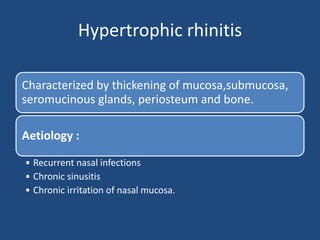
This document discusses acute and chronic rhinitis. It defines rhinitis and rhinosinusitis. For acute rhinitis, it describes viral, bacterial, and irritative types including common cold, influenza, diphtheritic rhinitis. For chronic rhinitis it distinguishes between specific types caused by infections/diseases and non-specific types including chronic simple rhinitis, hypertrophic rhinitis, atrophic rhinitis, rhinitis sicca, and rhinitis caseosa. It provides details on causes, symptoms, complications, and treatments for each type.