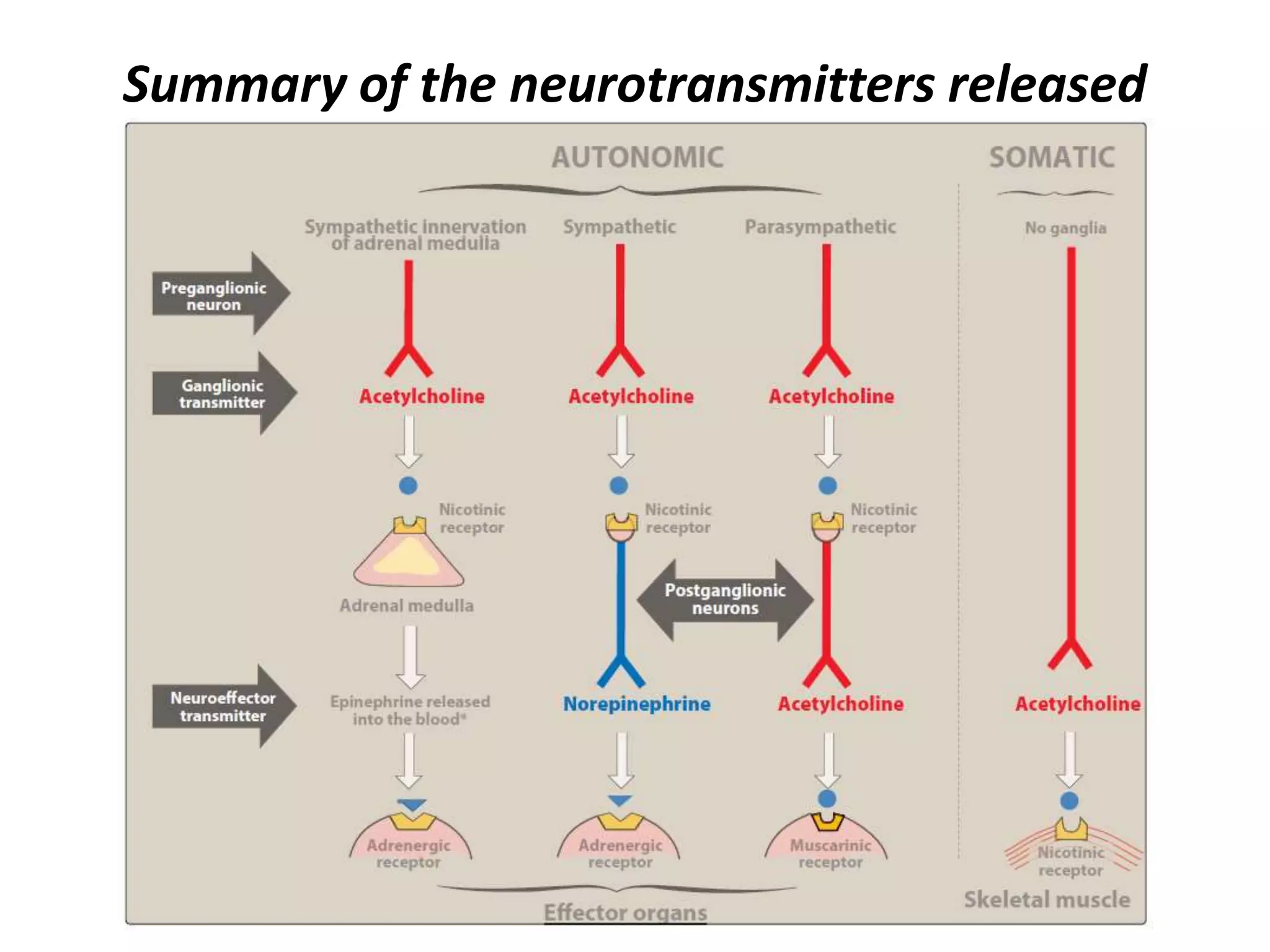
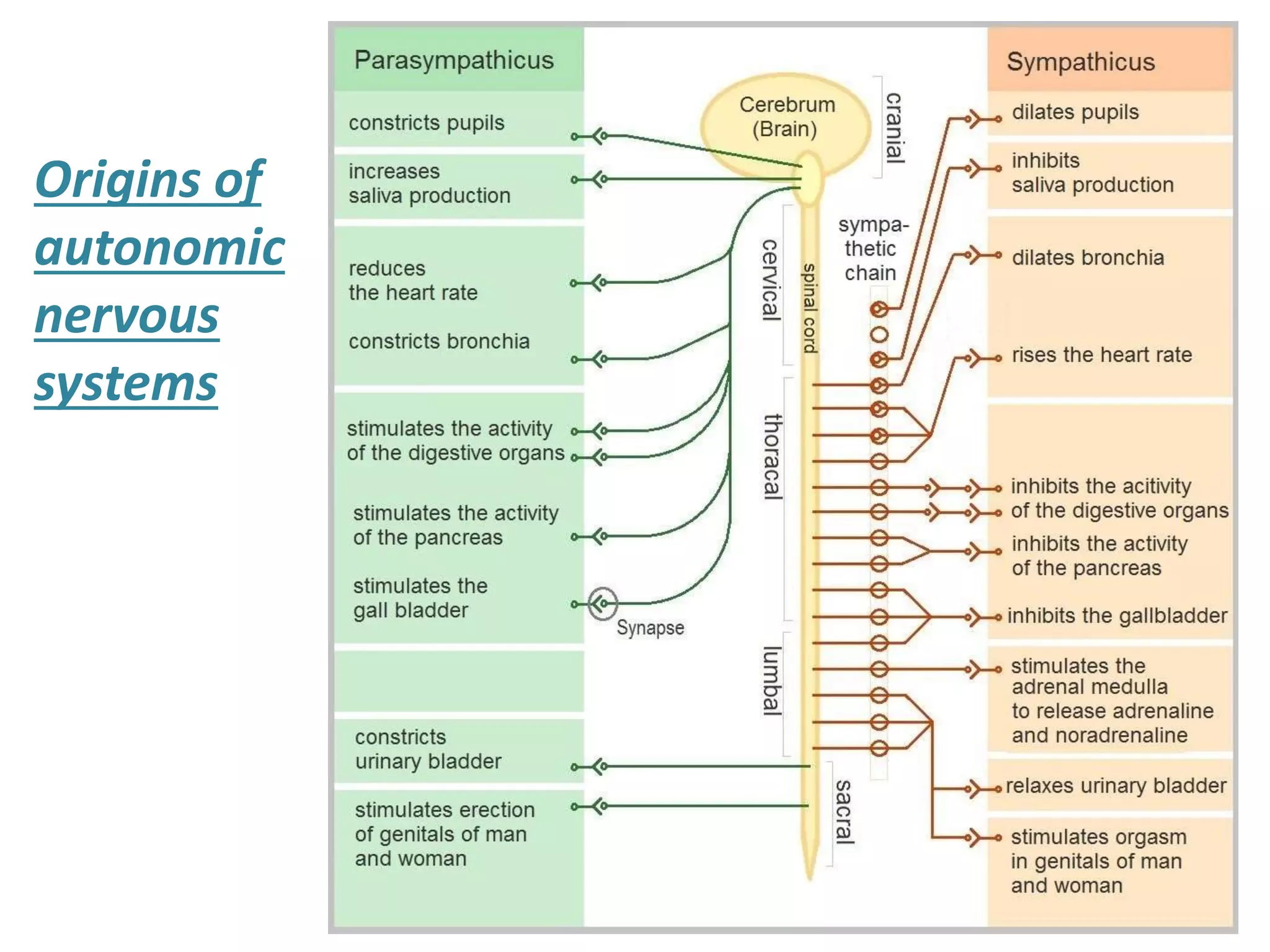
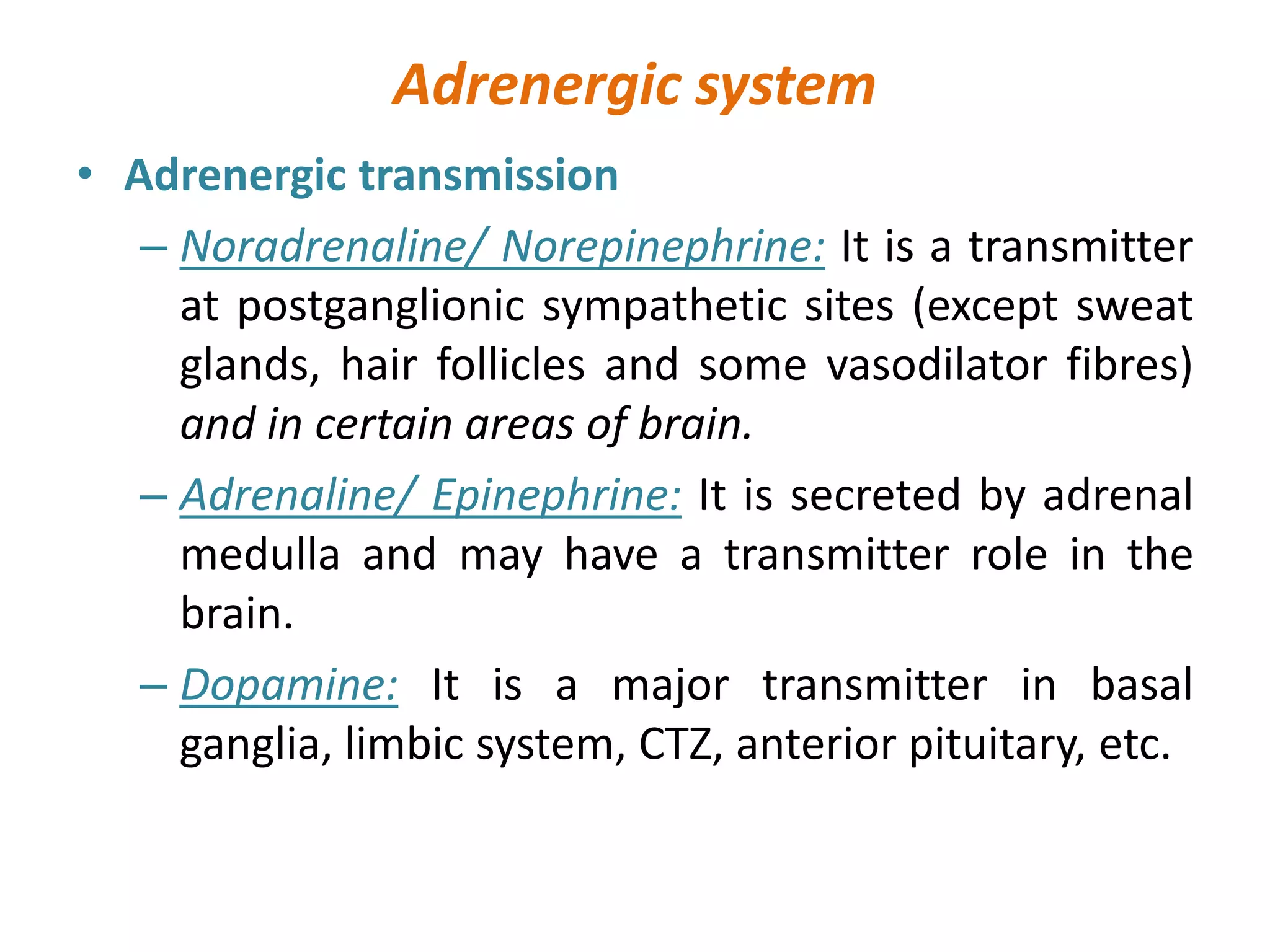
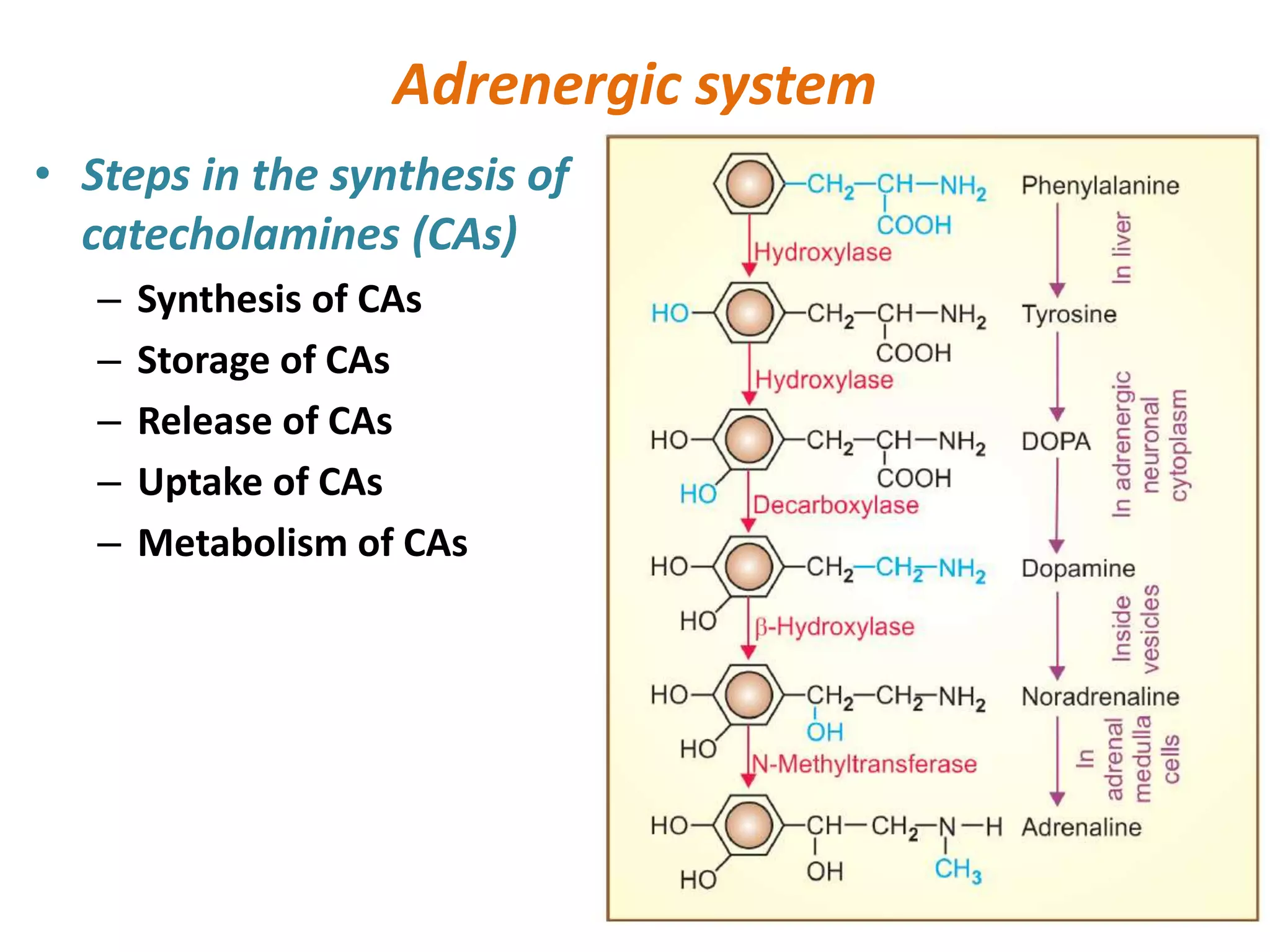
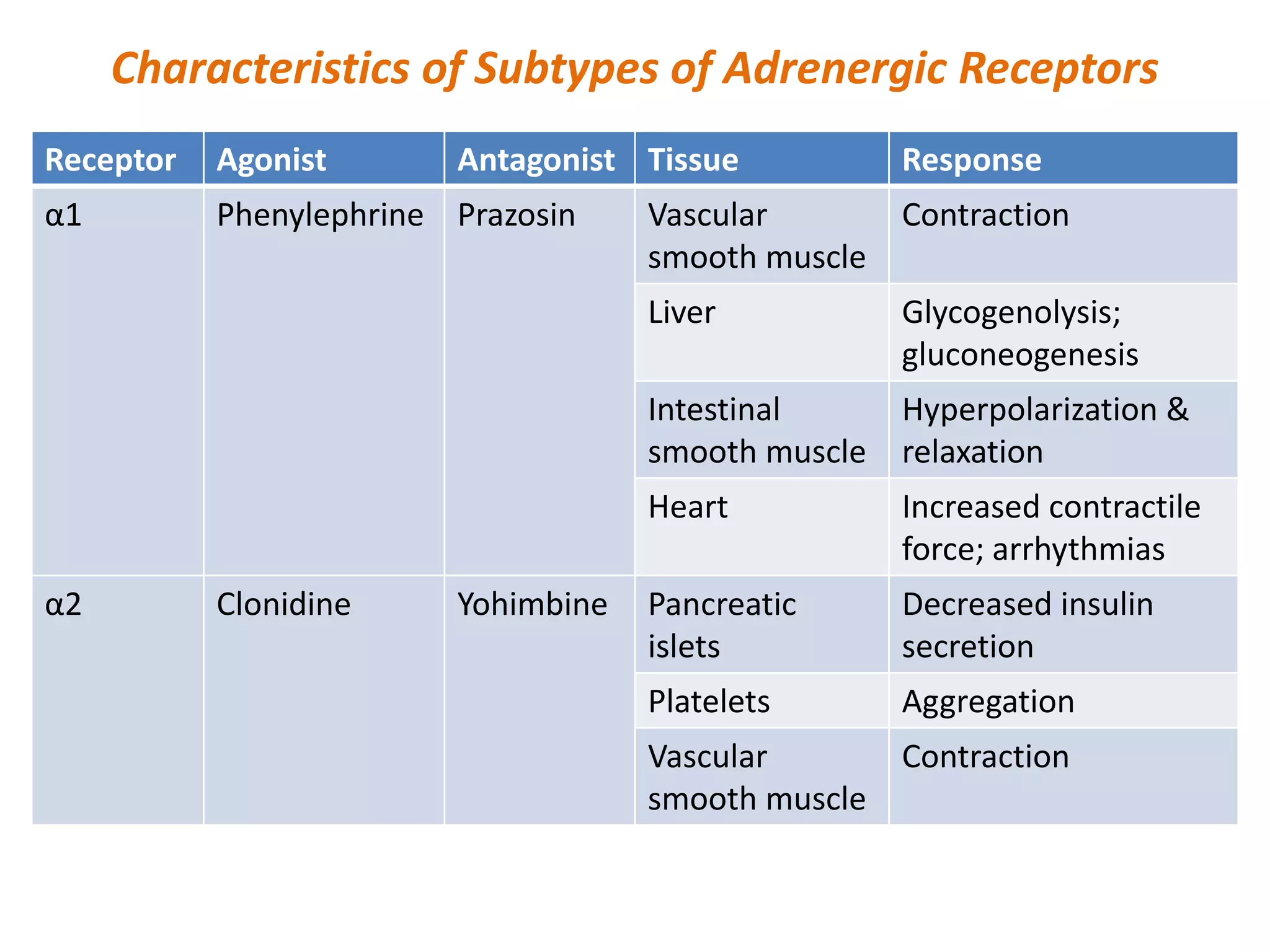
This document discusses the adrenergic system. It describes the origins and divisions of the autonomic nervous system, including the sympathetic and parasympathetic systems. It then focuses on the adrenergic system, summarizing the neurotransmitters involved, including norepinephrine, epinephrine, and dopamine. It outlines the steps in catecholamine synthesis, storage, release, reuptake, and metabolism. It also describes the different types of adrenergic receptors, including alpha and beta receptors, and provides examples of agonists and antagonists for each. Finally, it categorizes different types of adrenergic drugs.