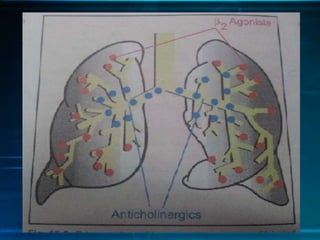
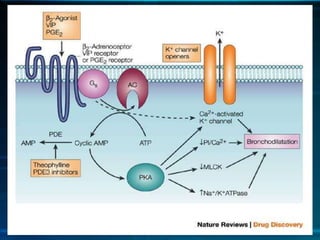
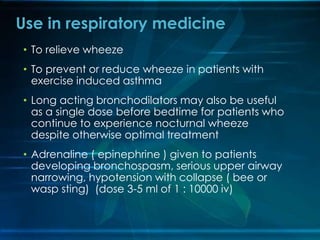
- Bronchodilators like epinephrine, salbutamol, and terbutaline work by binding to beta-2 receptors in the lungs, relaxing smooth muscle and dilating airways. They have been used for thousands of years to treat respiratory conditions.
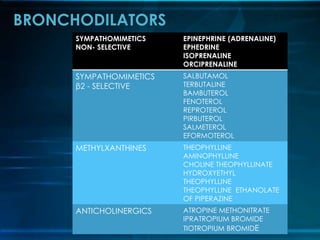
- Sympathomimetic bronchodilators are classified as non-selective or beta-2 selective. Non-selective drugs like epinephrine activate both alpha and beta receptors and are more likely to cause side effects, while beta-2 selective drugs primarily target the lungs.
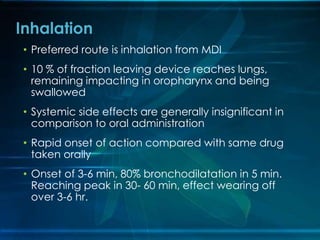
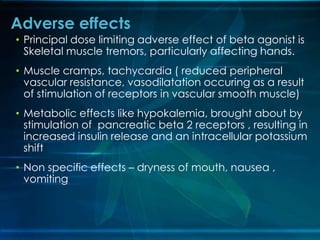
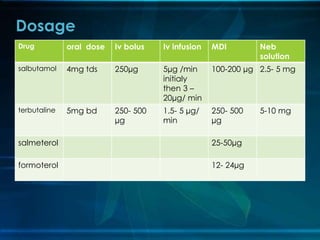
- Inhalation is the preferred route of administration as it delivers drugs directly to the lungs, but oral and intravenous routes can also be used. Common side effects include