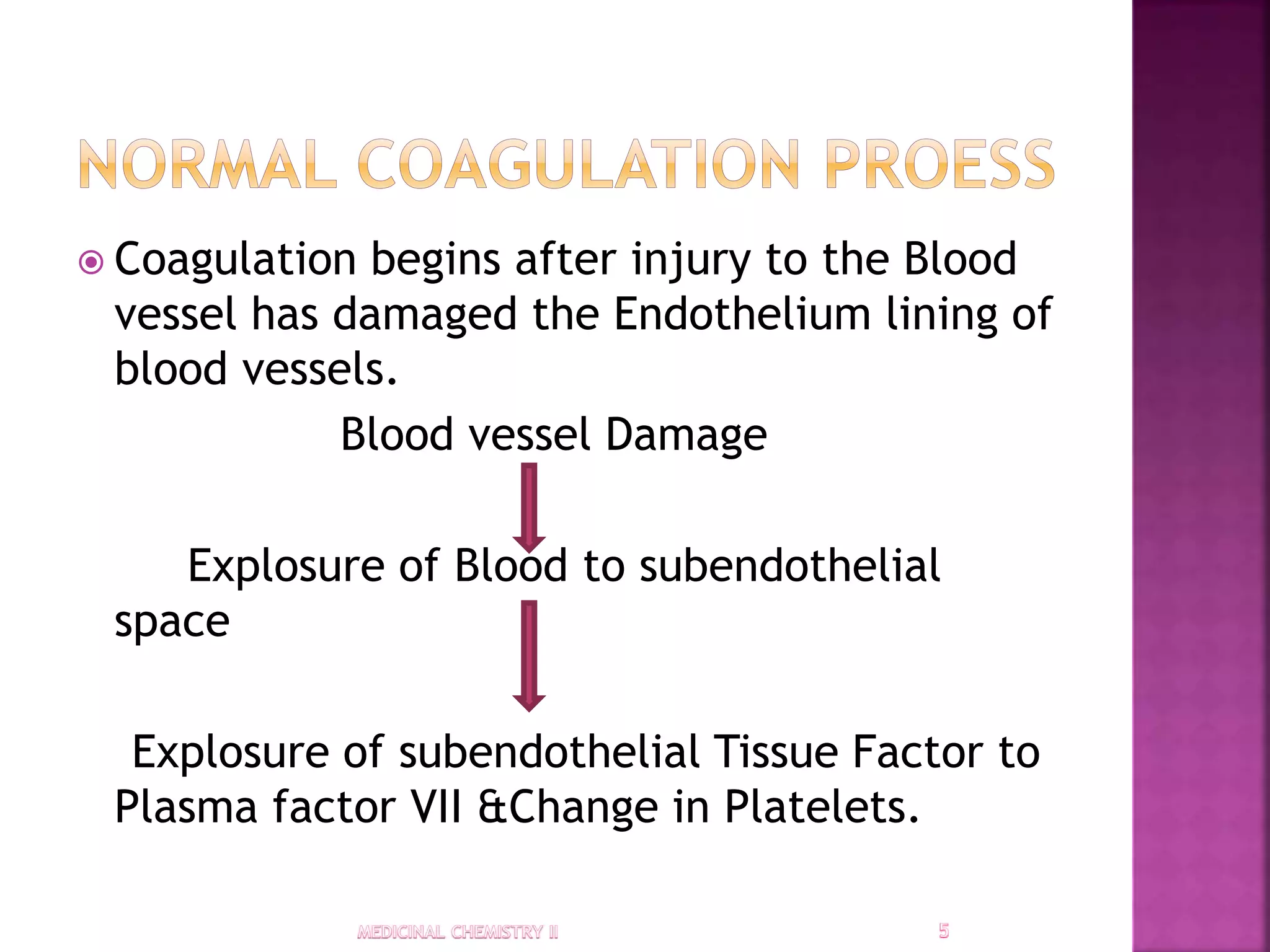
The document discusses the coagulation process, highlighting the formation of blood clots through primary and secondary hemostasis, and the roles of various coagulation factors and platelets. It also provides an overview of anticoagulants, including heparin and newer agents, their mechanisms of action, and indications for use in conditions like strokes and heart attacks. Additionally, it addresses the importance of antifibrinolytics and other drugs that affect platelet aggregation.