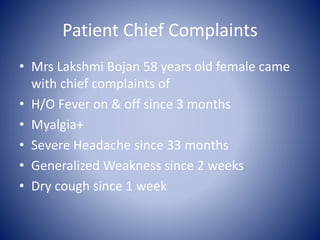
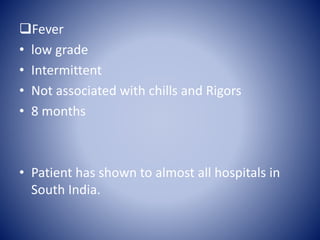
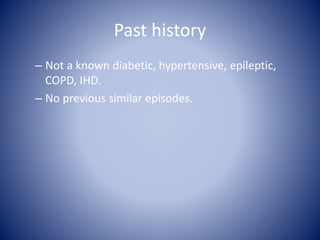
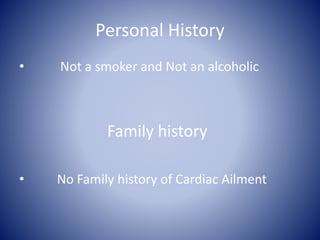
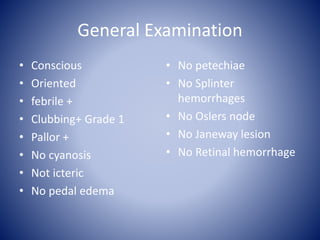
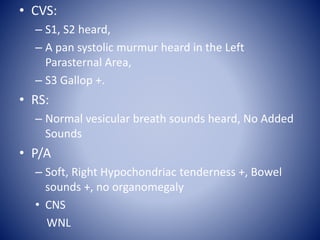
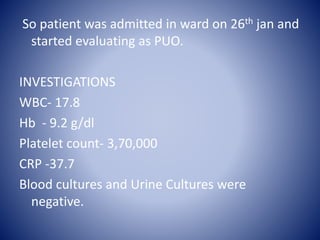
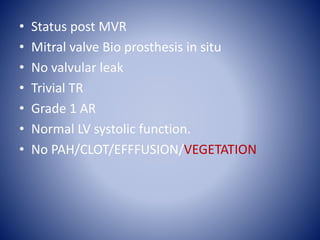
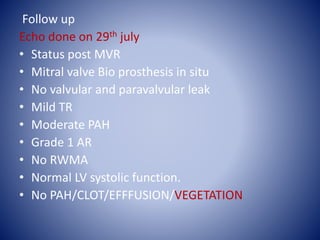
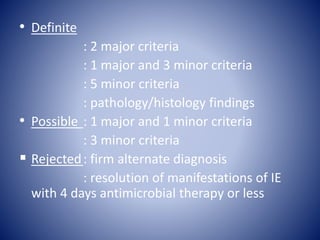
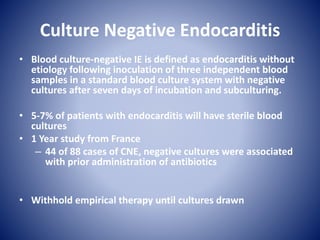
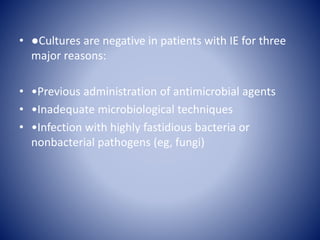
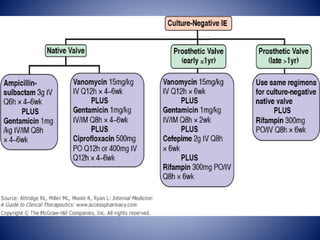
This case presentation describes a 58-year-old female patient who presented with fever, myalgia, severe headaches, and generalized weakness. Investigations revealed anemia, elevated inflammatory markers, and a positive transesophageal echocardiogram showing mitral valve vegetation. The patient was diagnosed with infective endocarditis of the mitral valve and underwent mitral valve replacement surgery. The document then provides details on the definition, diagnosis, and treatment of infective endocarditis, including descriptions of the Duke criteria for diagnosis and appropriate antibiotic therapy based on the infecting organism.