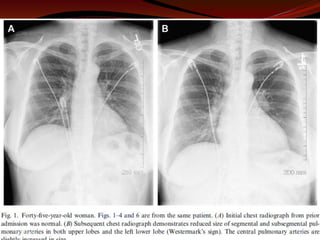
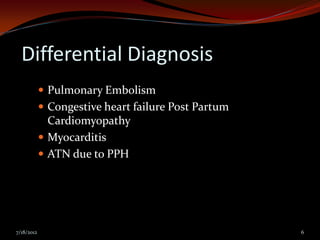
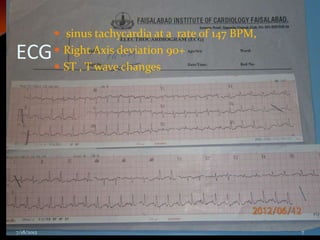
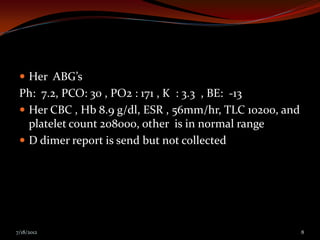
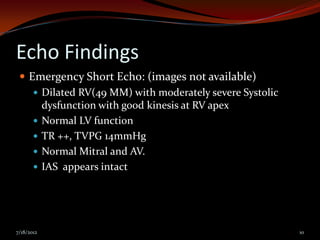
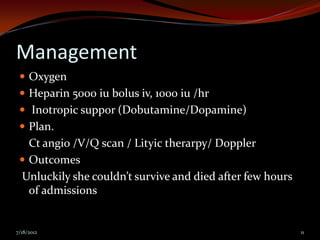
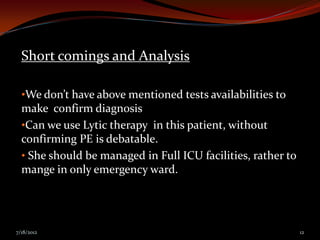
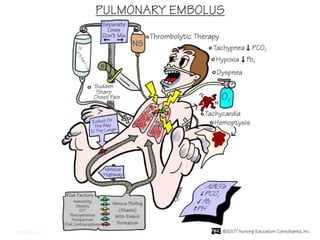
A 25-year-old female presented with severe shortness of breath that began suddenly. She had a normal vaginal delivery one week prior and mild shortness of breath for three days after. On examination, she was tachycardic, tachypneic, and hypoxic. Echocardiogram showed right ventricular dysfunction. She was diagnosed with pulmonary embolism but died after a few hours despite treatment. The case presentation discusses a young female diagnosed with pulmonary embolism after childbirth who died despite emergency treatment.
![Clinical Presentation
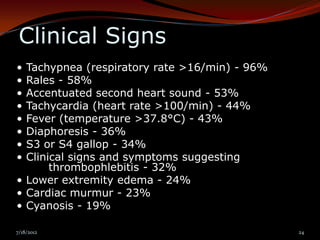
The PIOPED study reported the following
incidence of common symptoms of pulmonary
embolism[30] :
• Dyspnea (73%)
• Pleuritic chest pain (66%)
• Cough (37%)
• Hemoptysis (13%) Symptoms
7/18/2012 23](https://image.slidesharecdn.com/pulmonaryemoblismbydryaser-120718135924-phpapp01/85/Pulmonary-emoblism-by-dr-yaser-23-320.jpg)