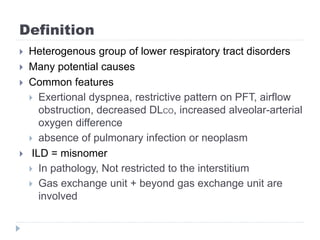
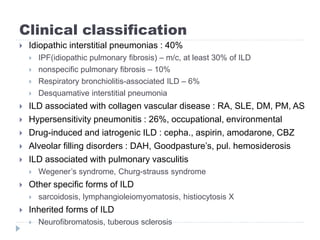
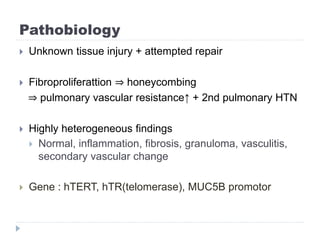
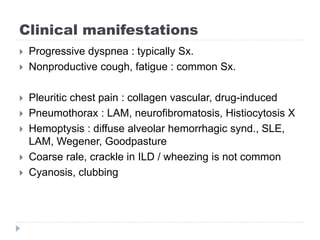
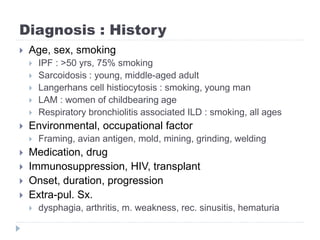
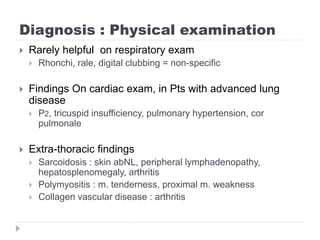
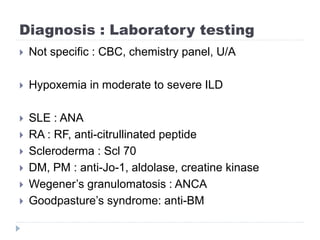
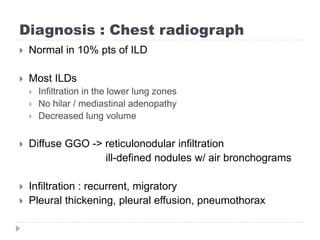
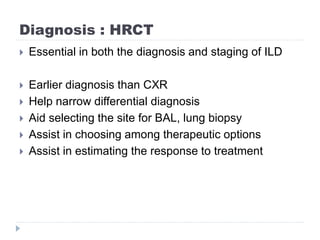
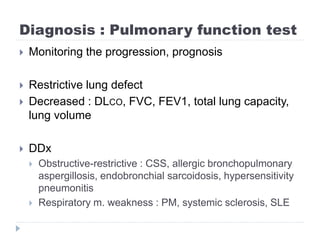
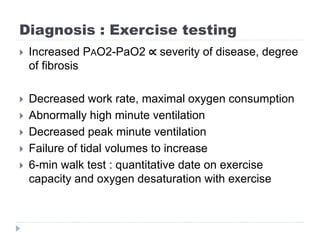
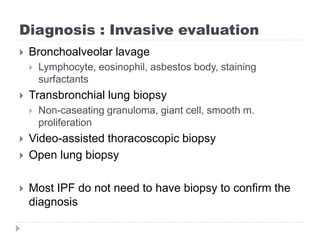
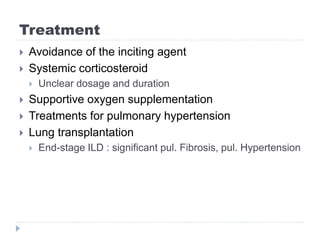
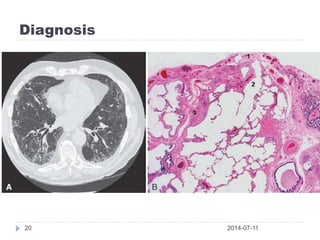
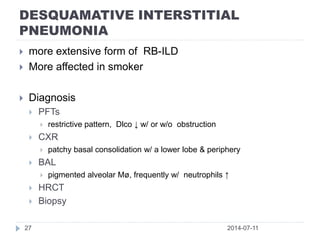
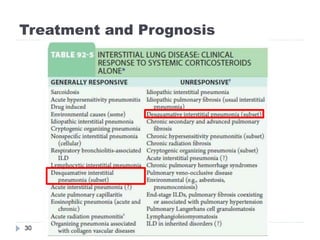
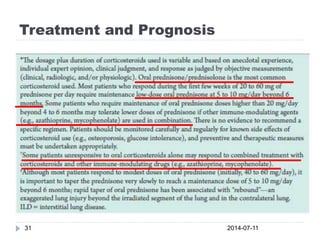
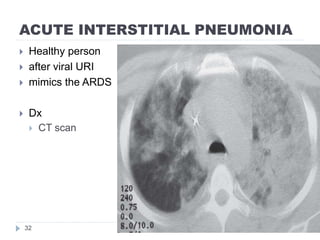
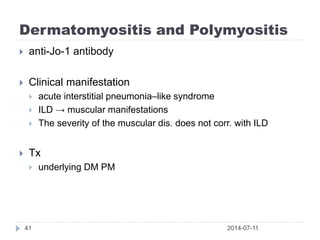
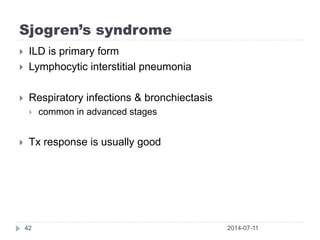
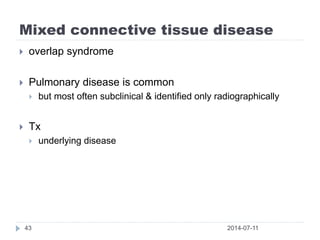
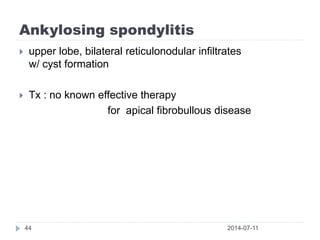
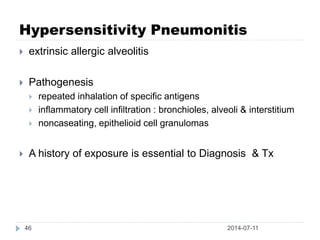
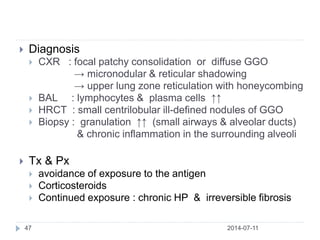
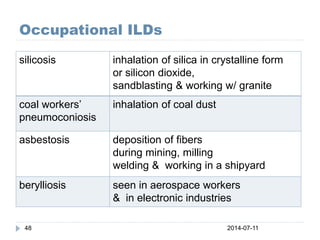
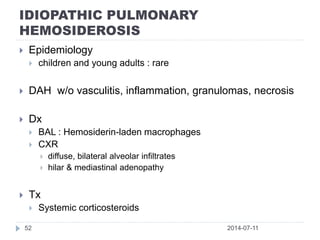
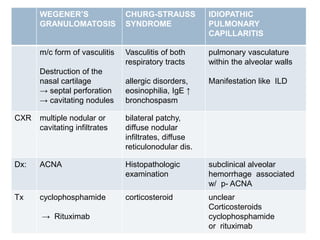
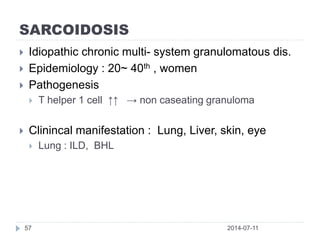
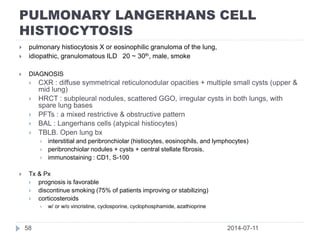
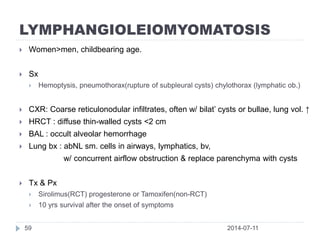
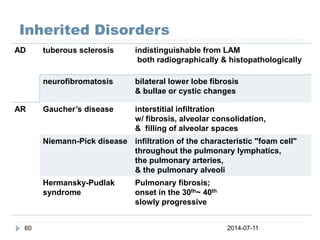
This document provides an overview of interstitial lung disease (ILD). ILD is a heterogeneous group of lower respiratory disorders with common features including dyspnea, restrictive lung patterns, and decreased gas exchange. The document discusses the clinical classification of ILD including idiopathic interstitial pneumonias like idiopathic pulmonary fibrosis, hypersensitivity pneumonitis, and ILD associated with collagen vascular diseases. Epidemiology, pathobiology, clinical manifestations, diagnostic workup, and treatment approaches for various forms of ILD are also summarized.