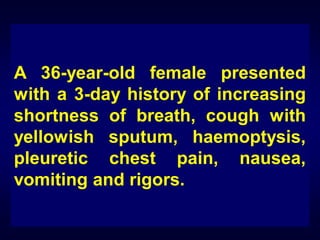
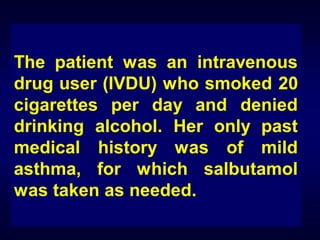
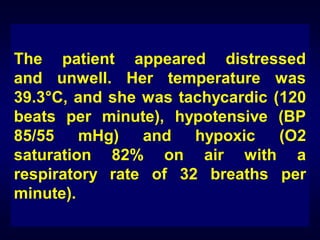
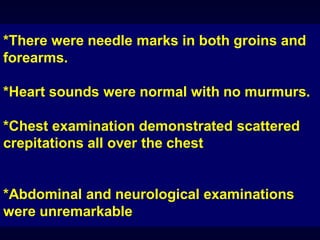
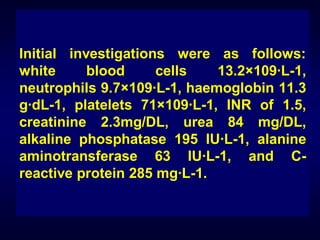
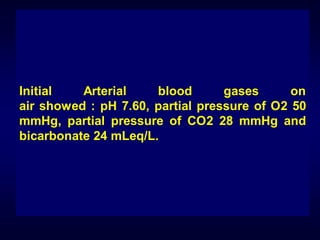
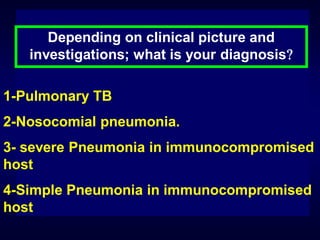
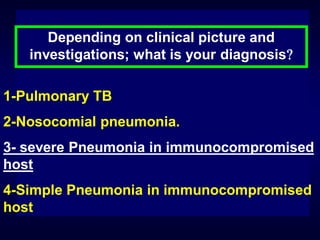
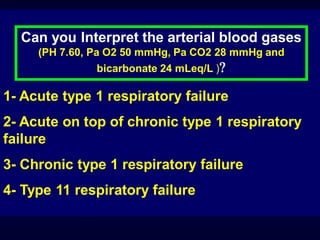
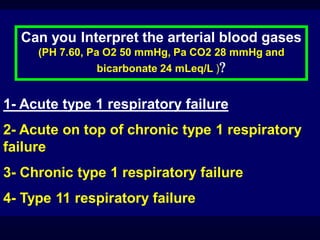
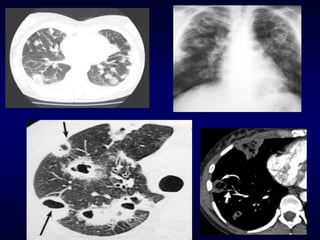
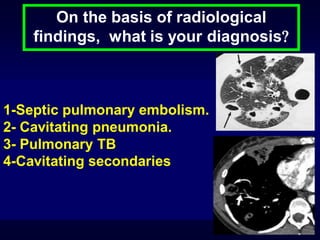
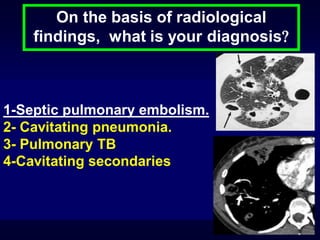
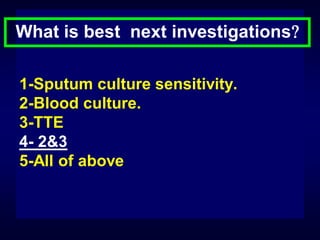
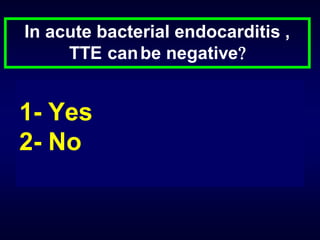
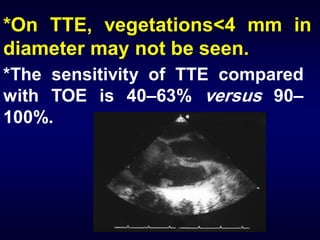
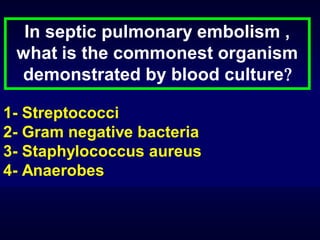
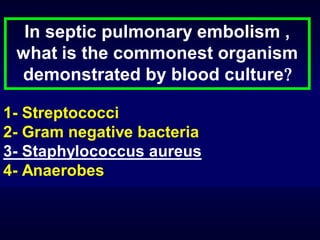
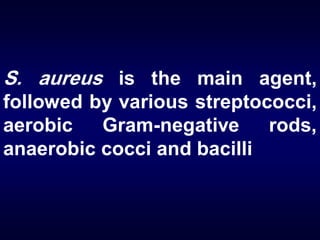
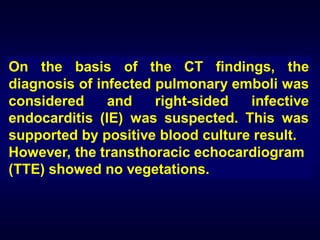
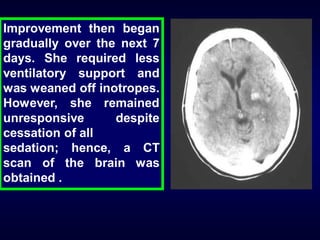
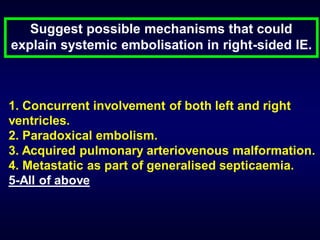
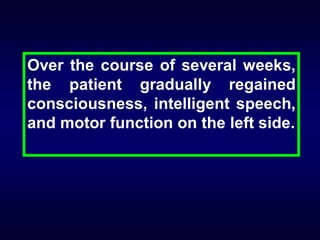
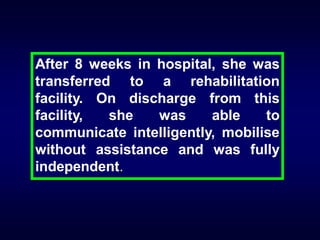
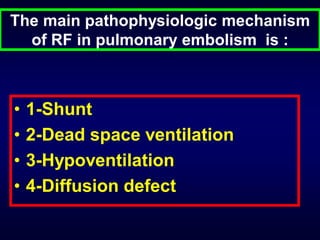
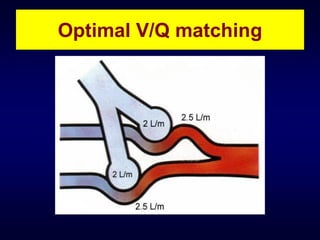
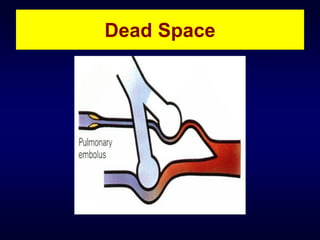
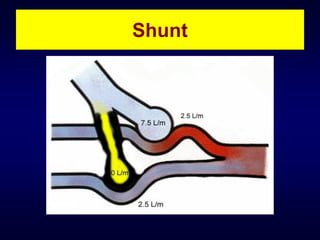
This case report describes a 36-year-old female intravenous drug user who presented with shortness of breath, cough, fever, and other symptoms. Clinical exams and tests showed signs of infection and respiratory failure. She was diagnosed with infected pulmonary emboli and suspected infective endocarditis. Despite treatment, her condition deteriorated and she developed multiple organ complications. Further scans revealed brain lesions. She gradually recovered over several weeks. Key learning points included the risks of endocarditis in intravenous drug users and challenges in diagnosis, as well as potential for full recovery despite severe sepsis and neurological damage.