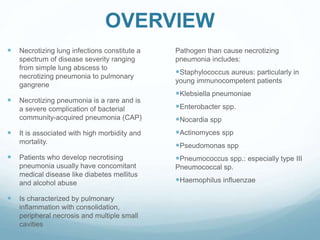
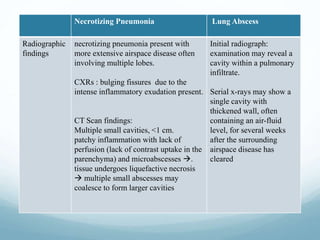
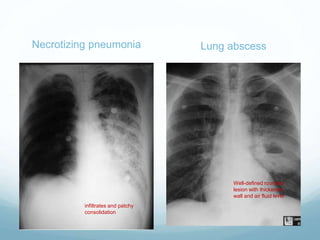
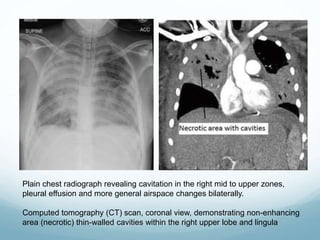
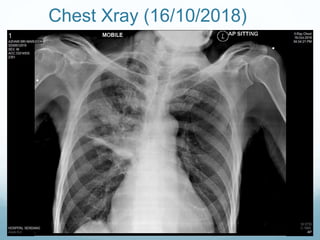
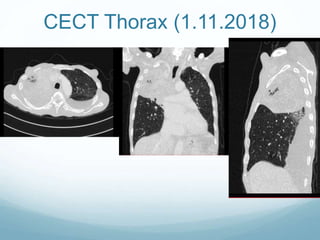
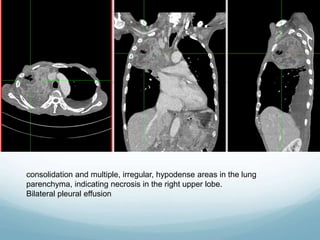
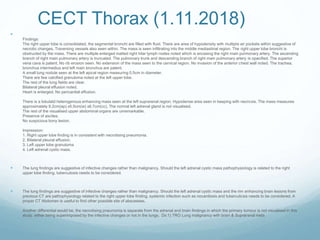
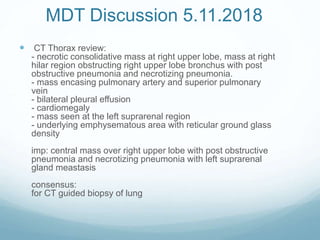
Necrotizing pneumonia is a rare and severe complication of bacterial community-acquired pneumonia that is associated with high morbidity and mortality. It is characterized by pulmonary inflammation, consolidation, peripheral necrosis, and multiple small cavities. A 62-year-old man with a history of tuberculosis and diabetes presented with fever, weakness, and respiratory failure. Imaging showed necrotizing pneumonia in the right upper lobe with multiple small cavities and abscesses. He deteriorated despite treatment and died from his illness.