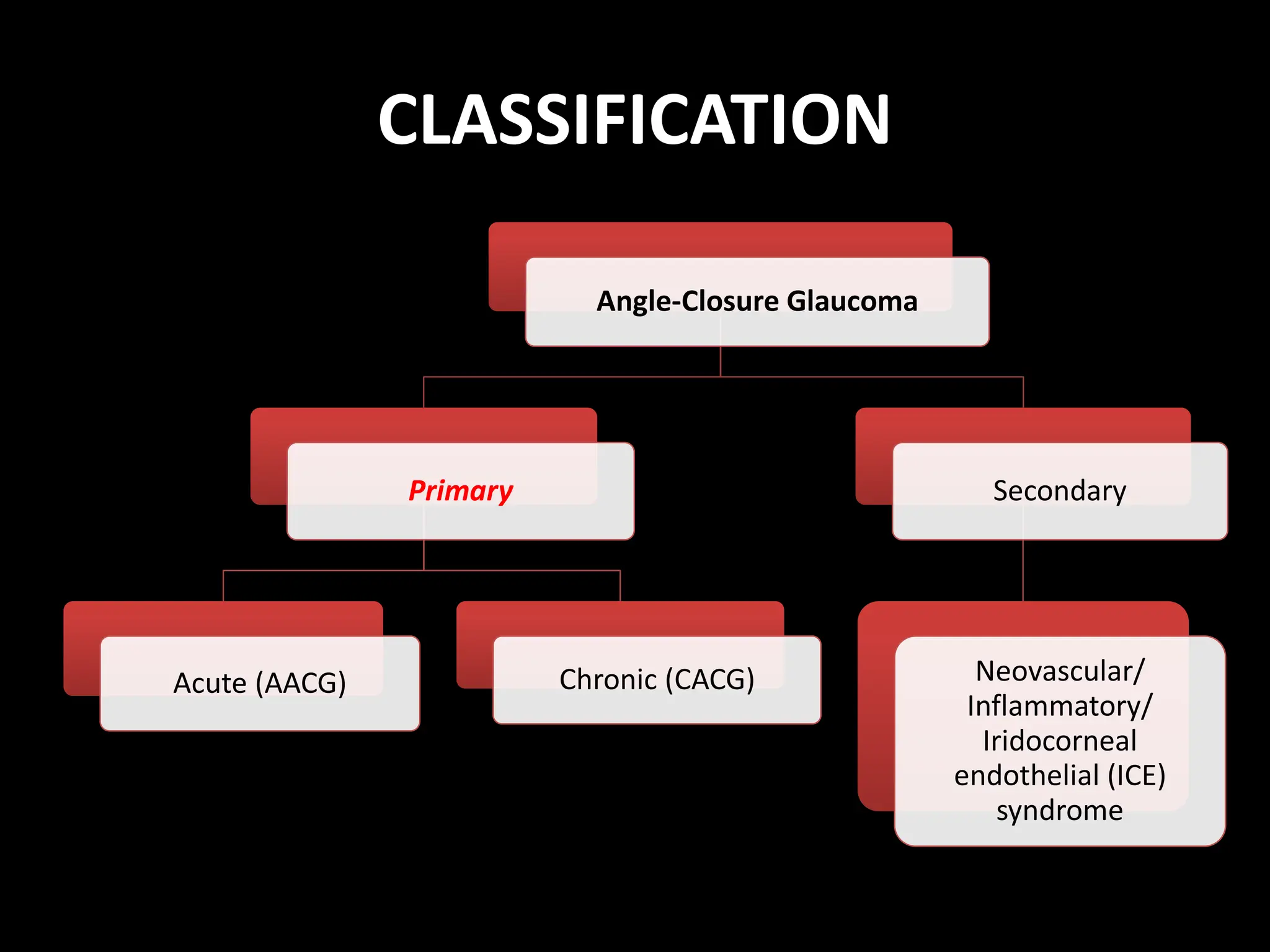
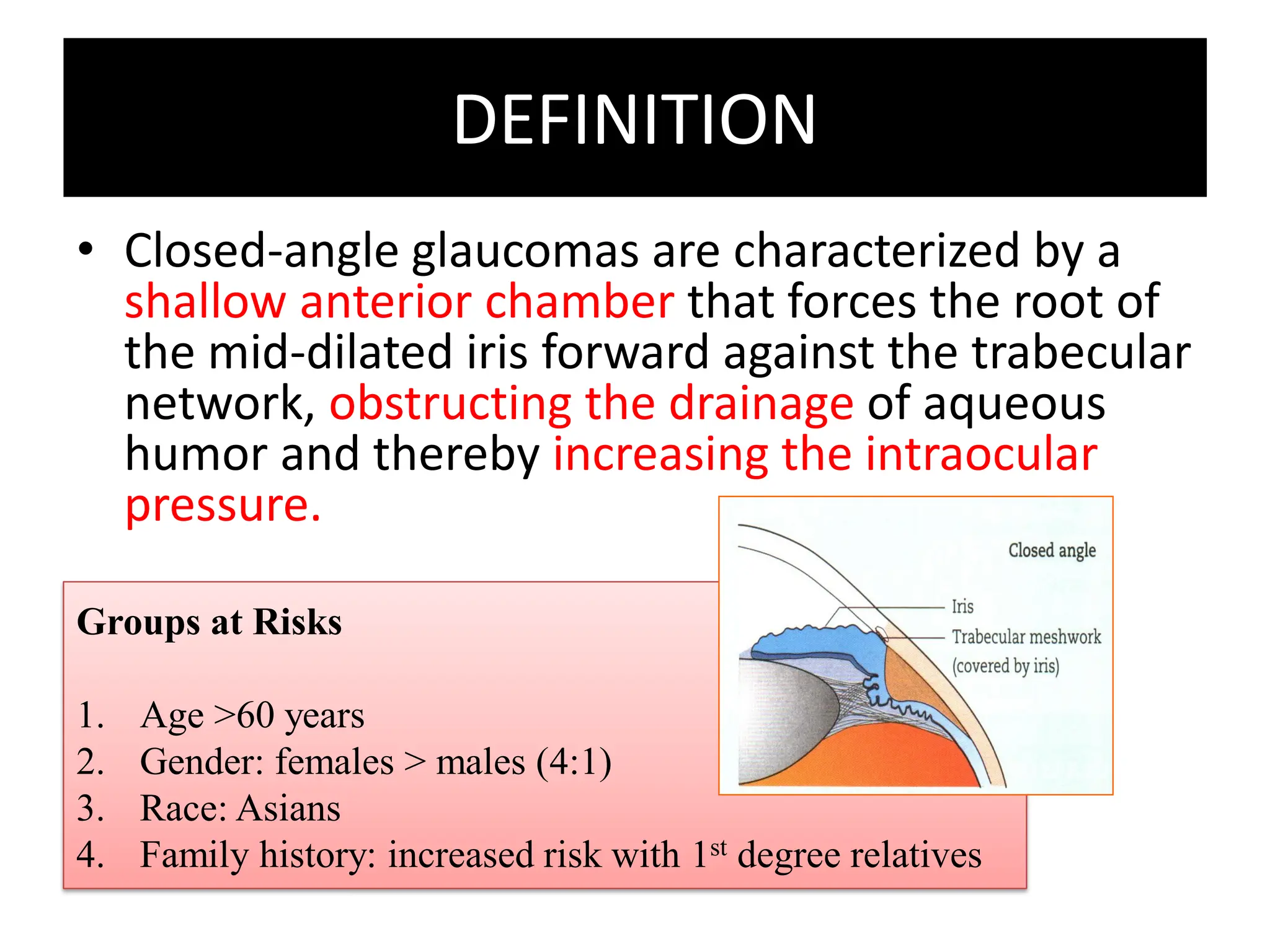
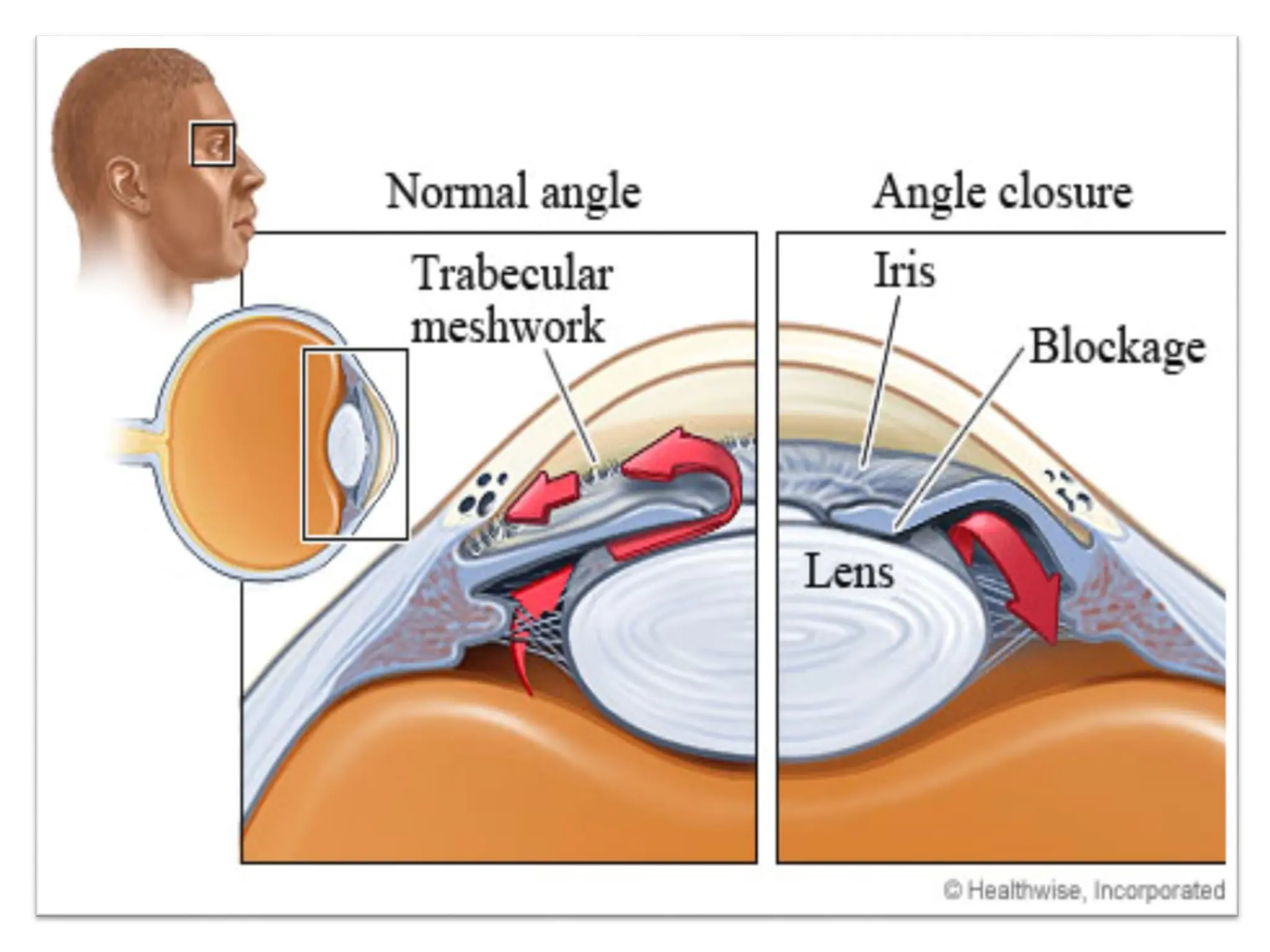
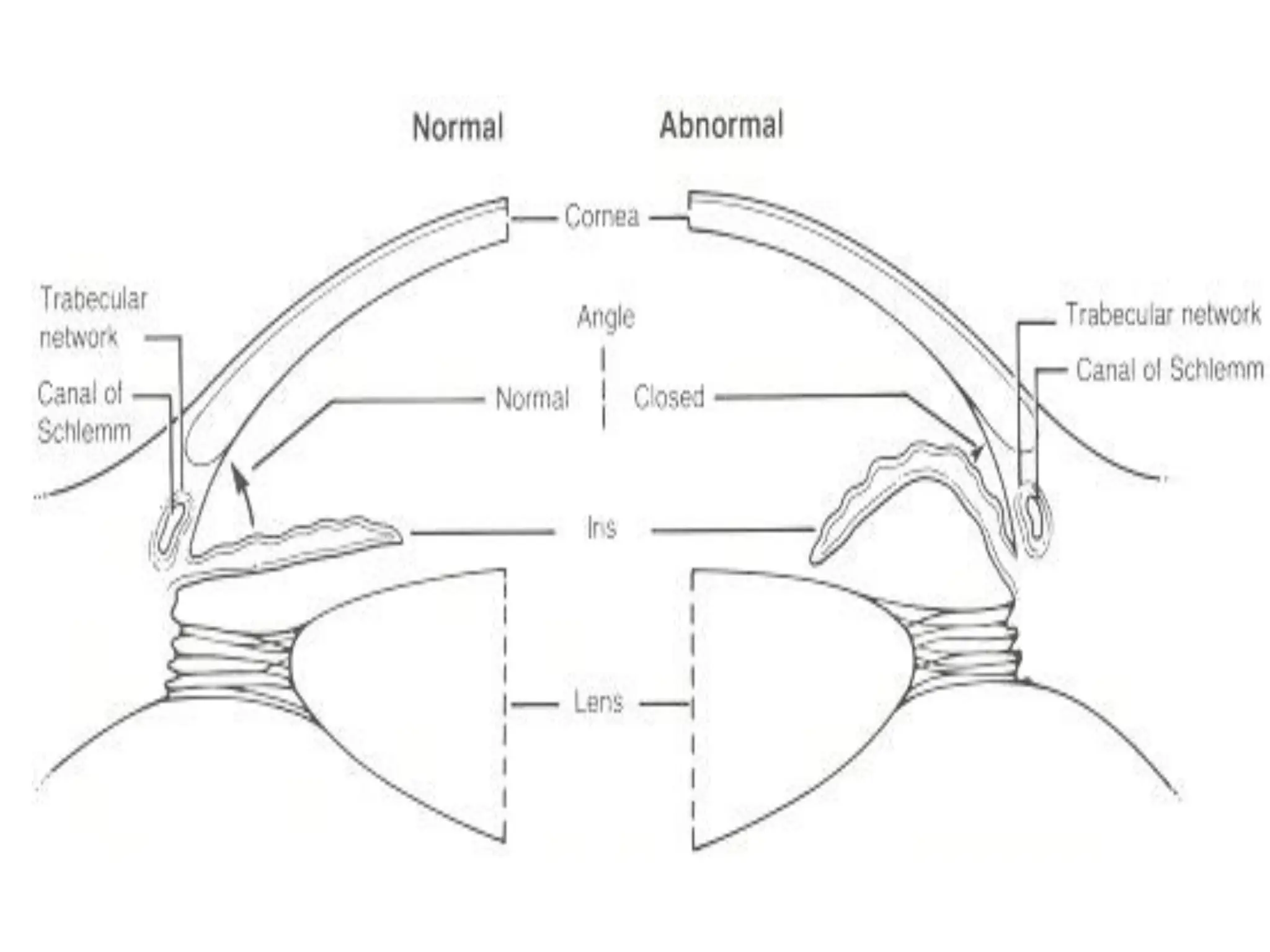
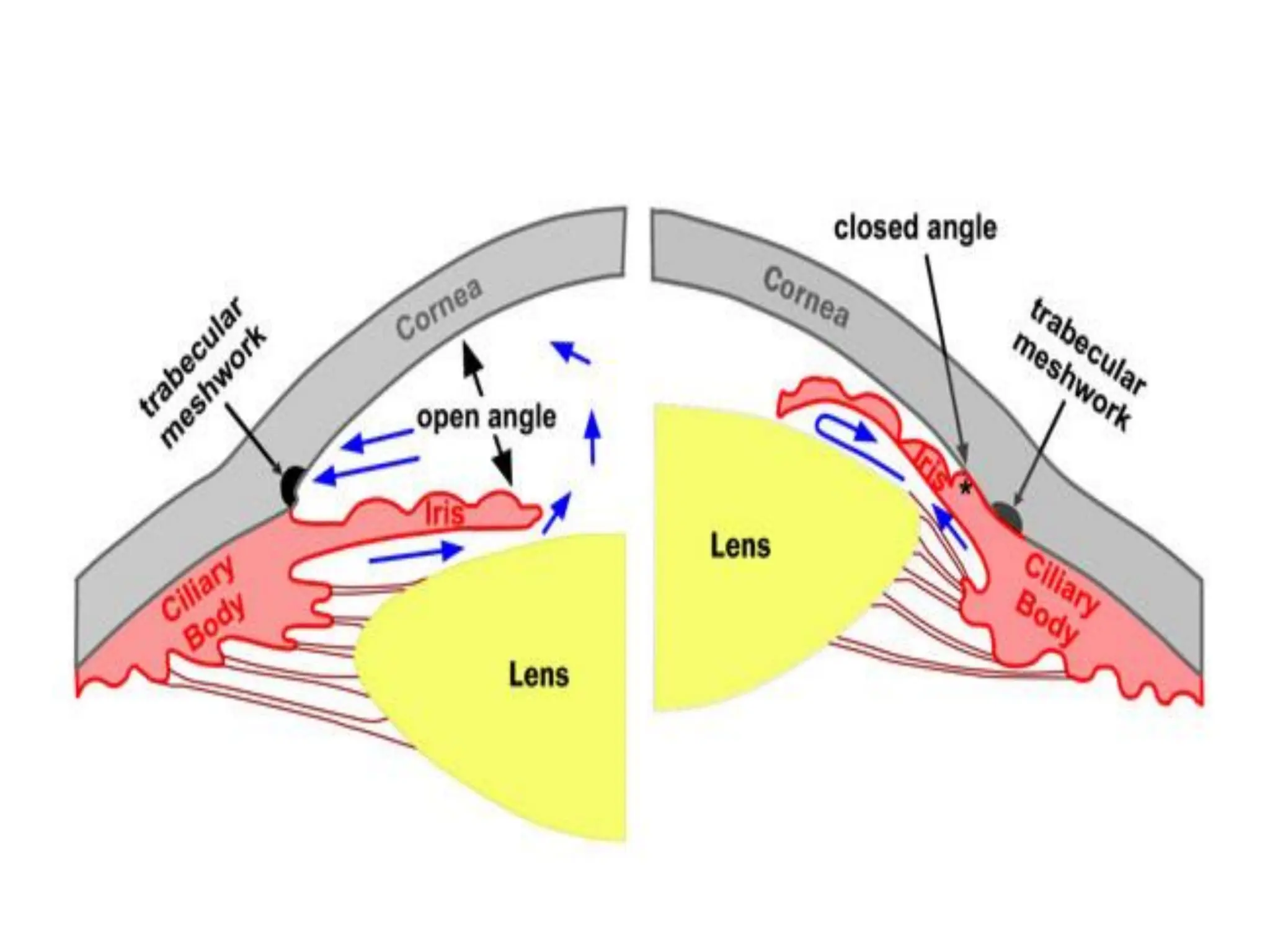
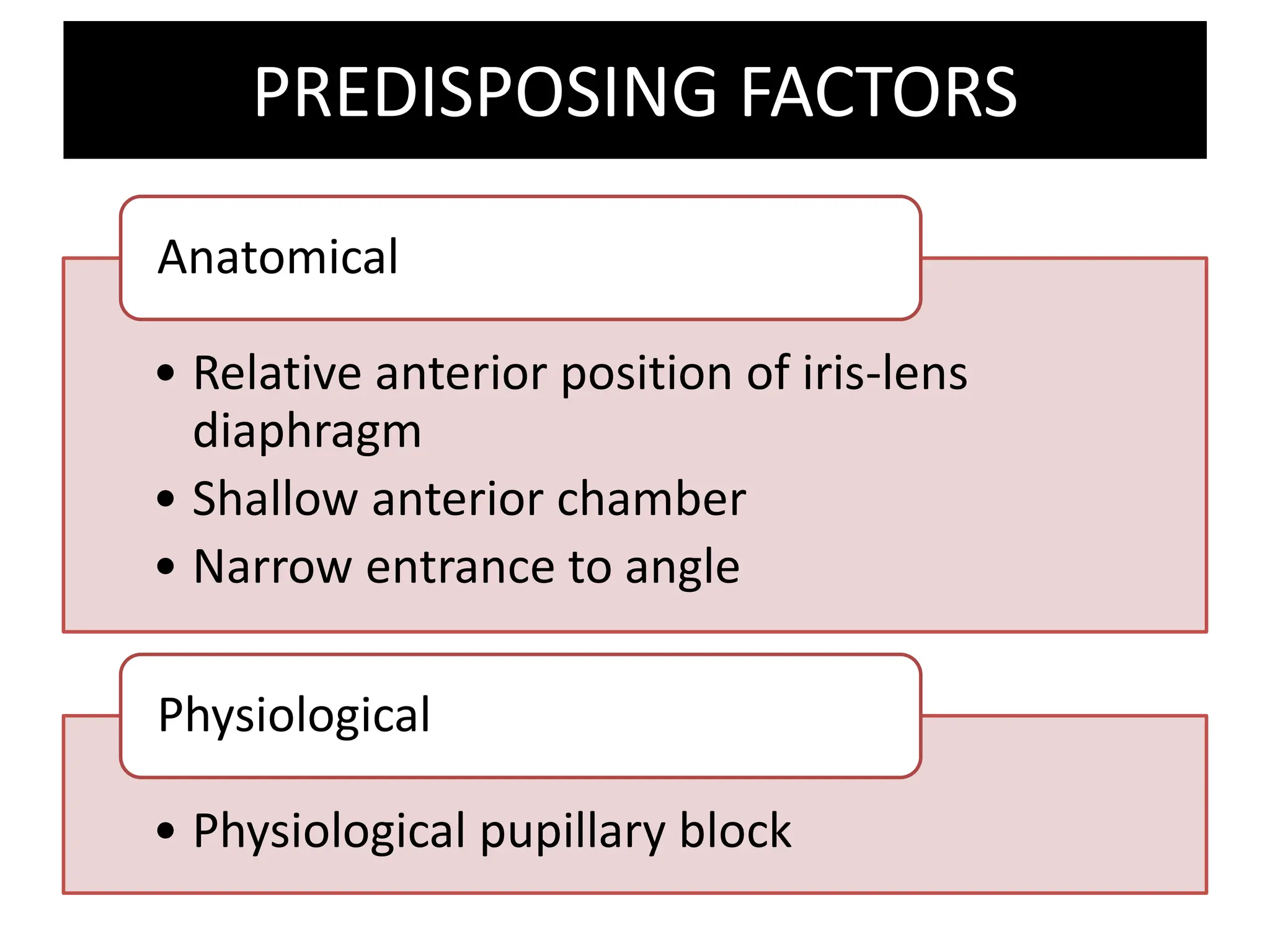
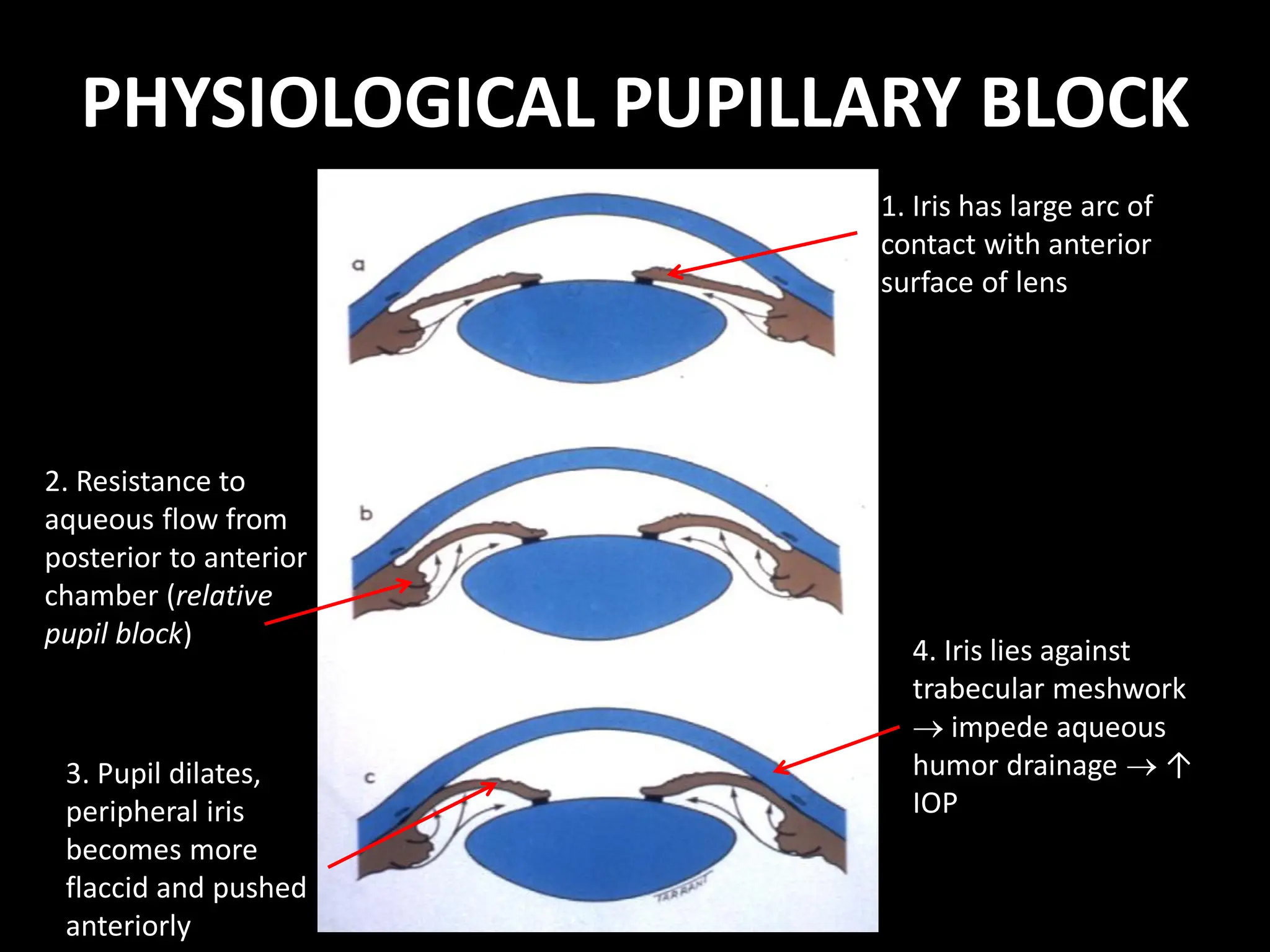
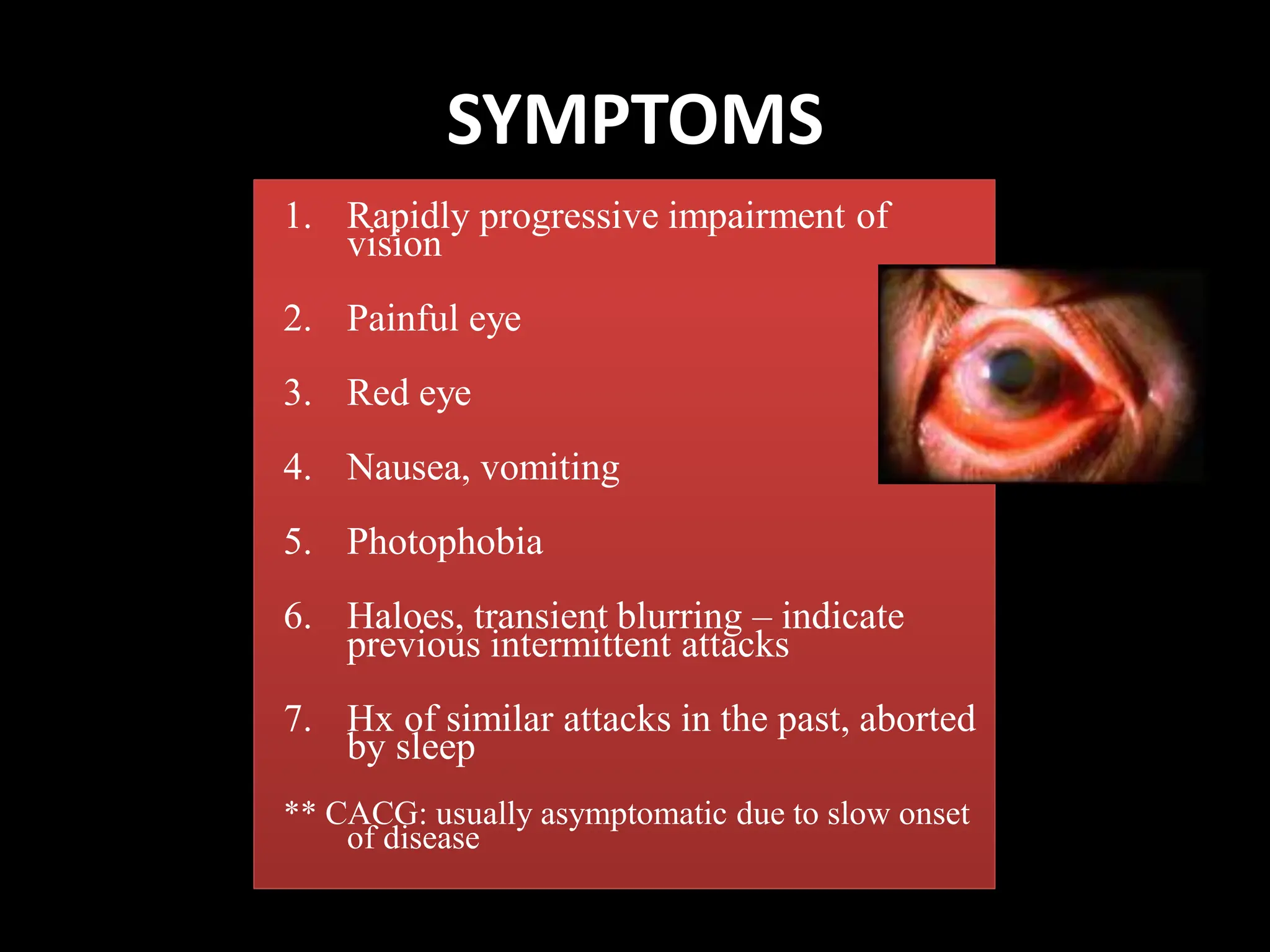
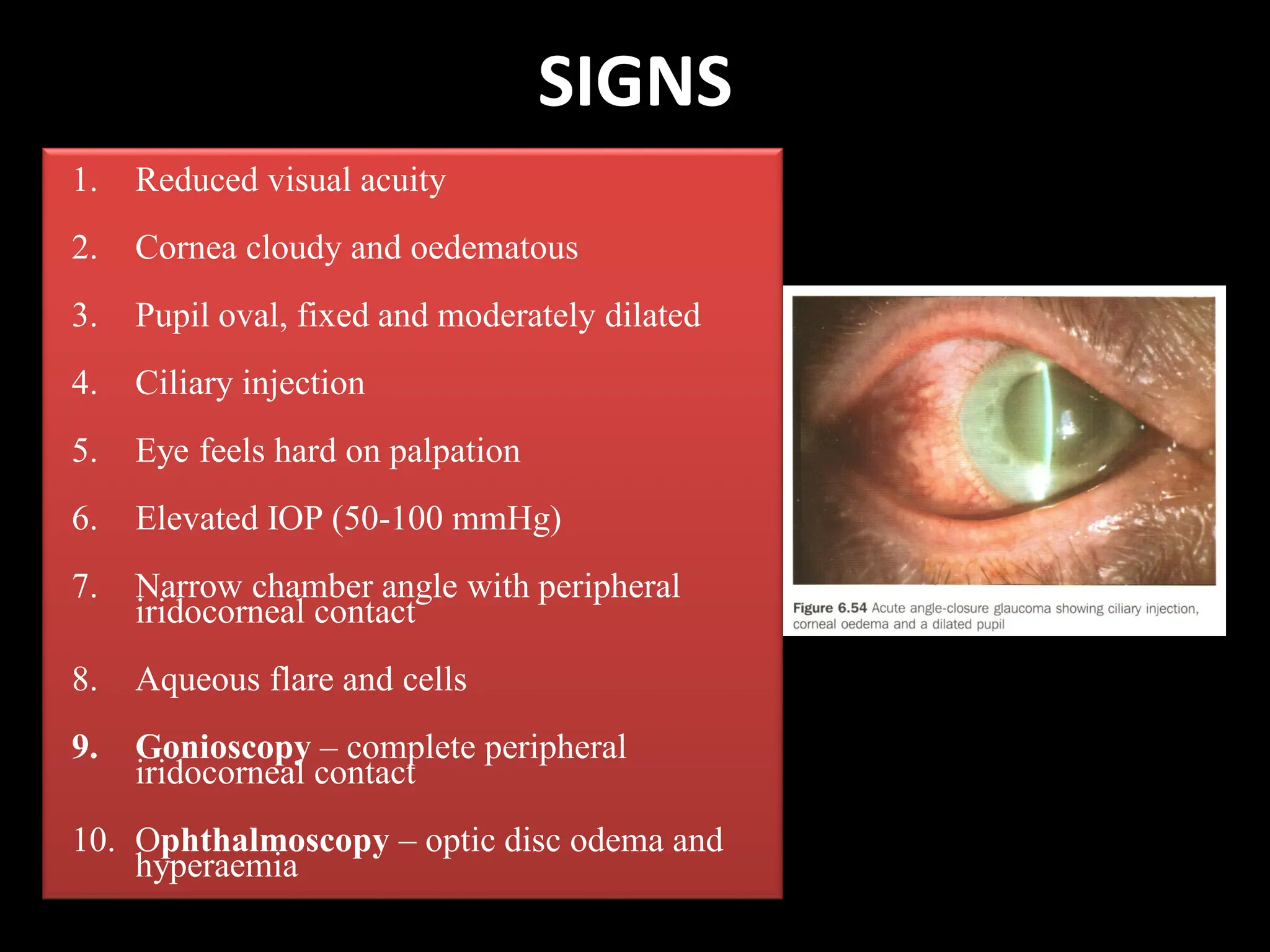
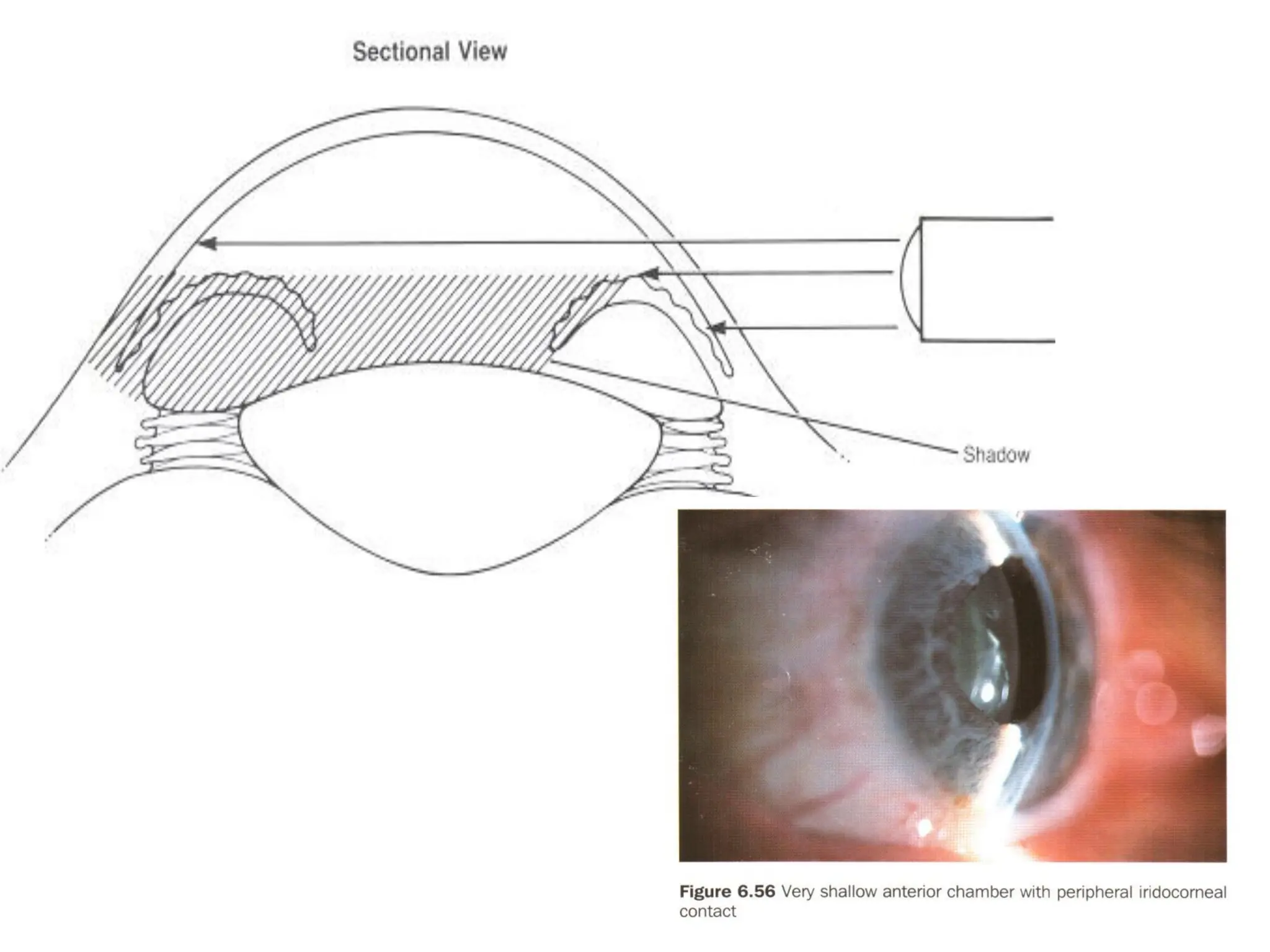
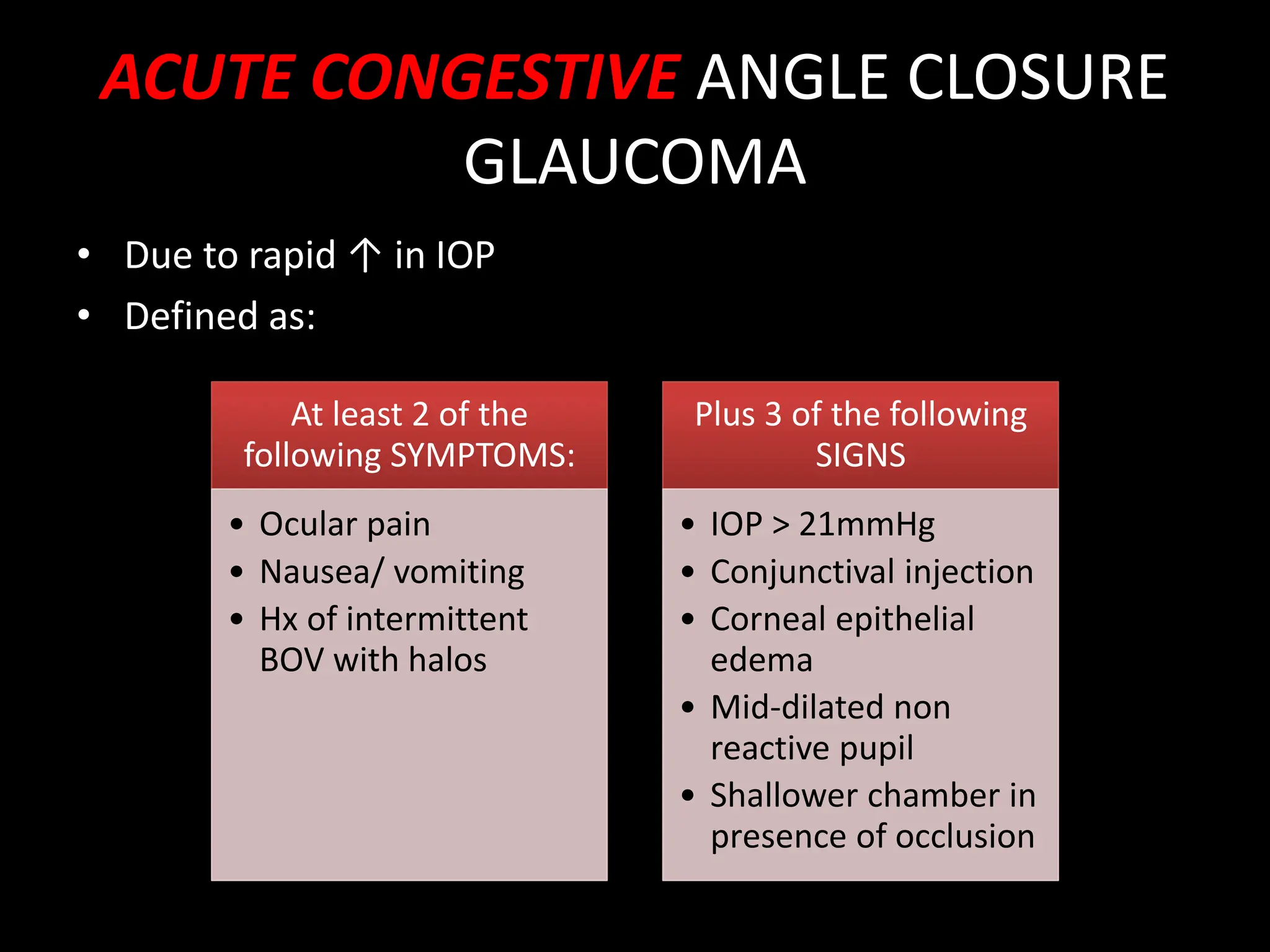
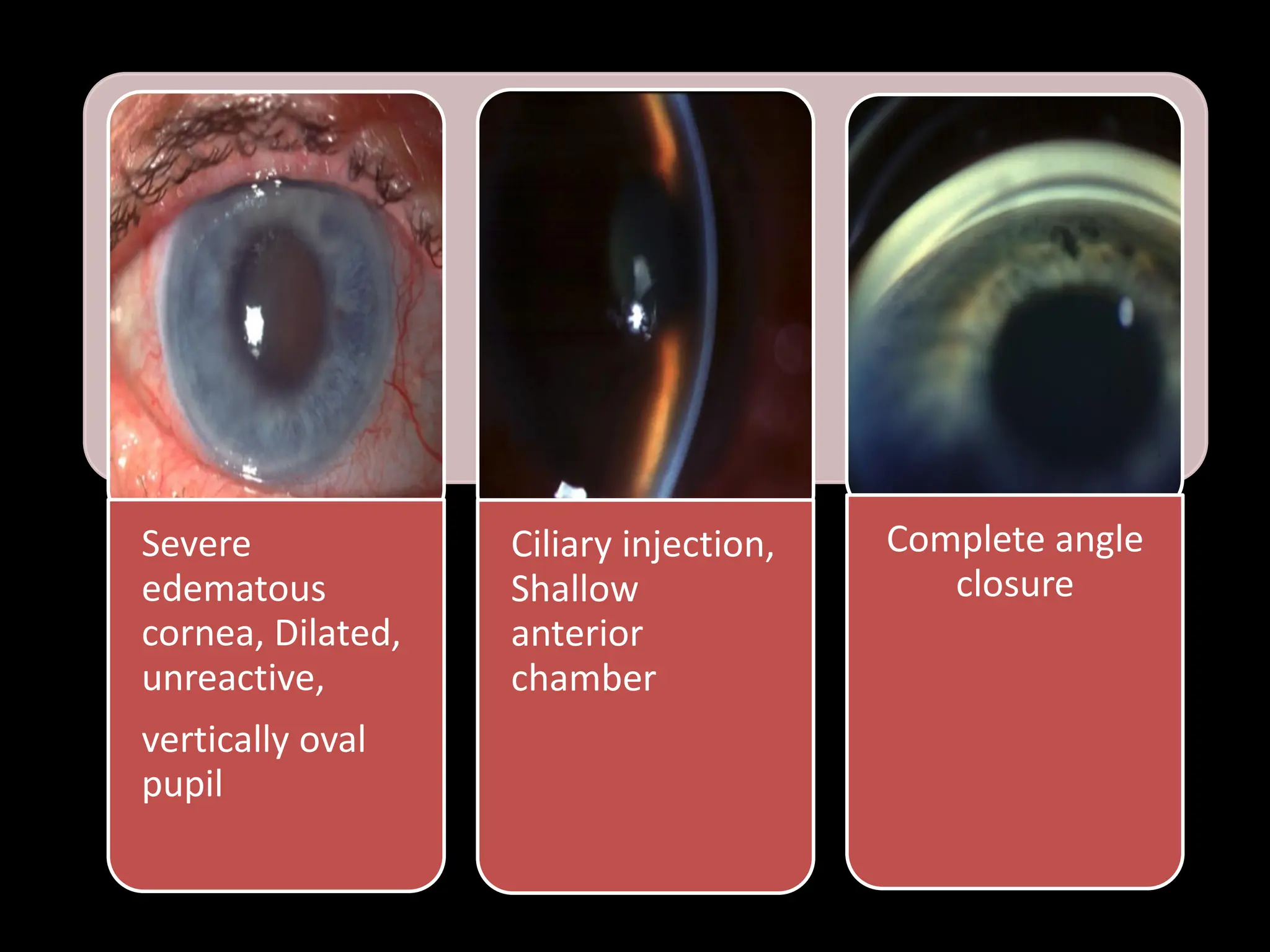
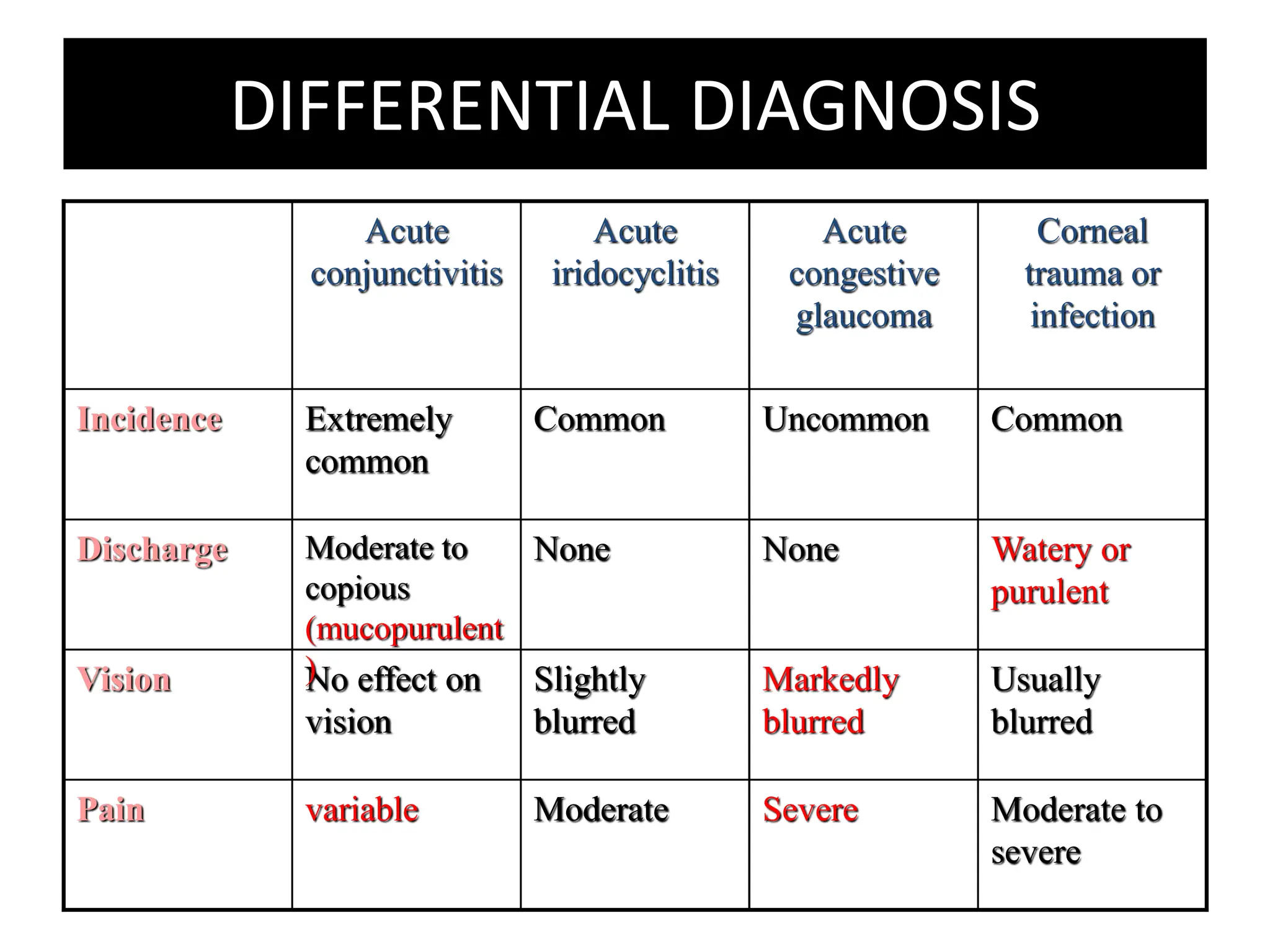
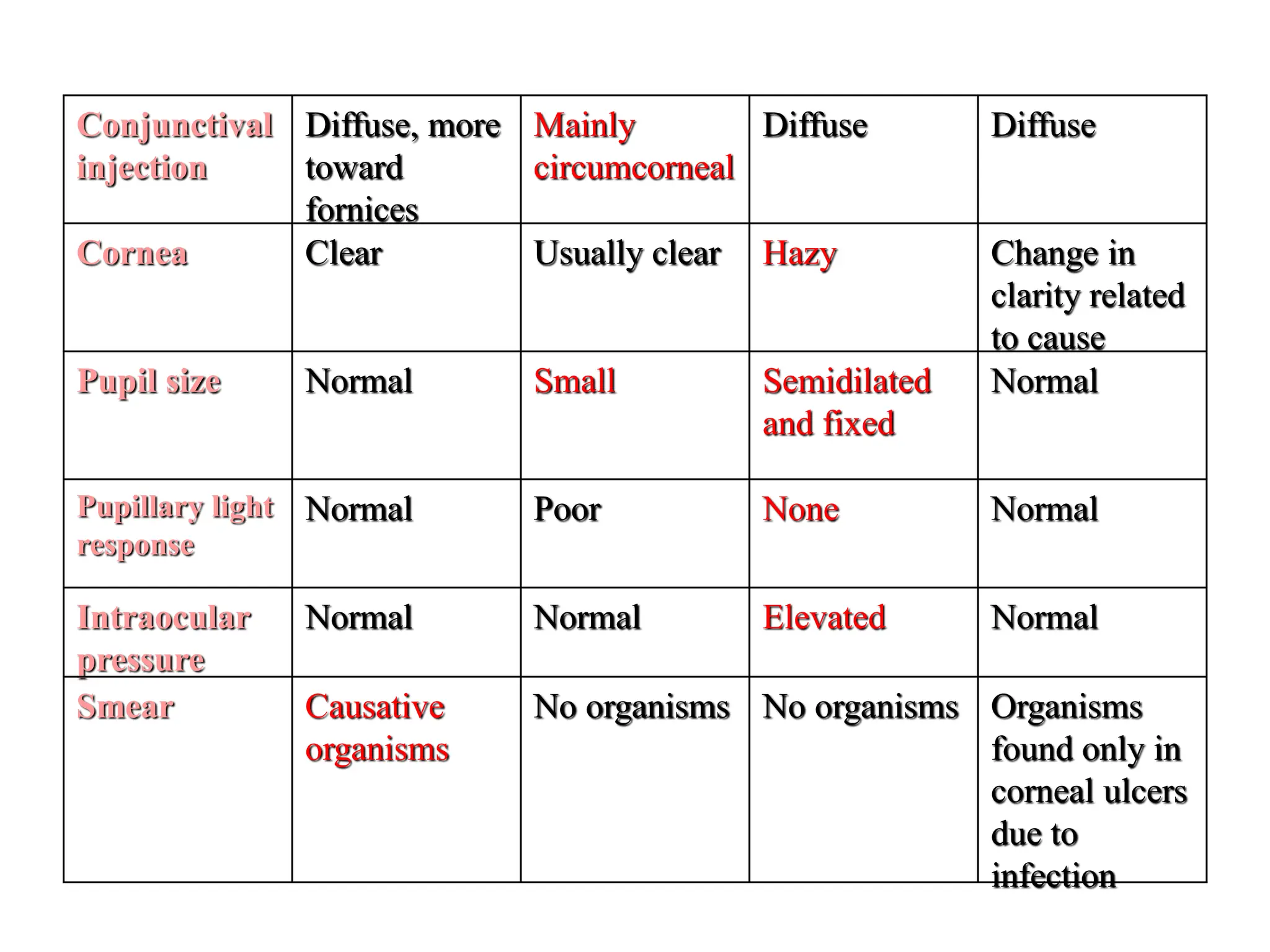
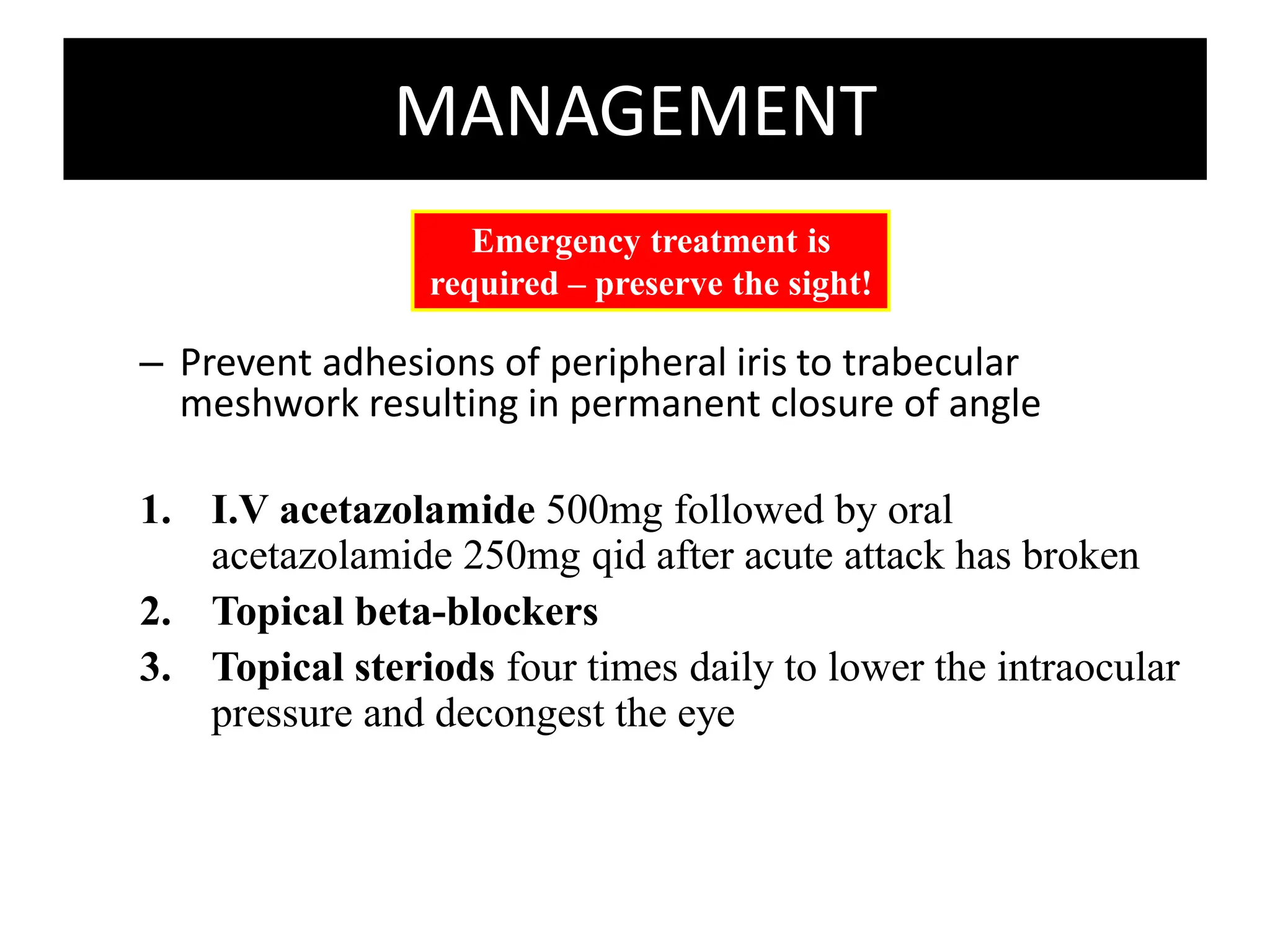
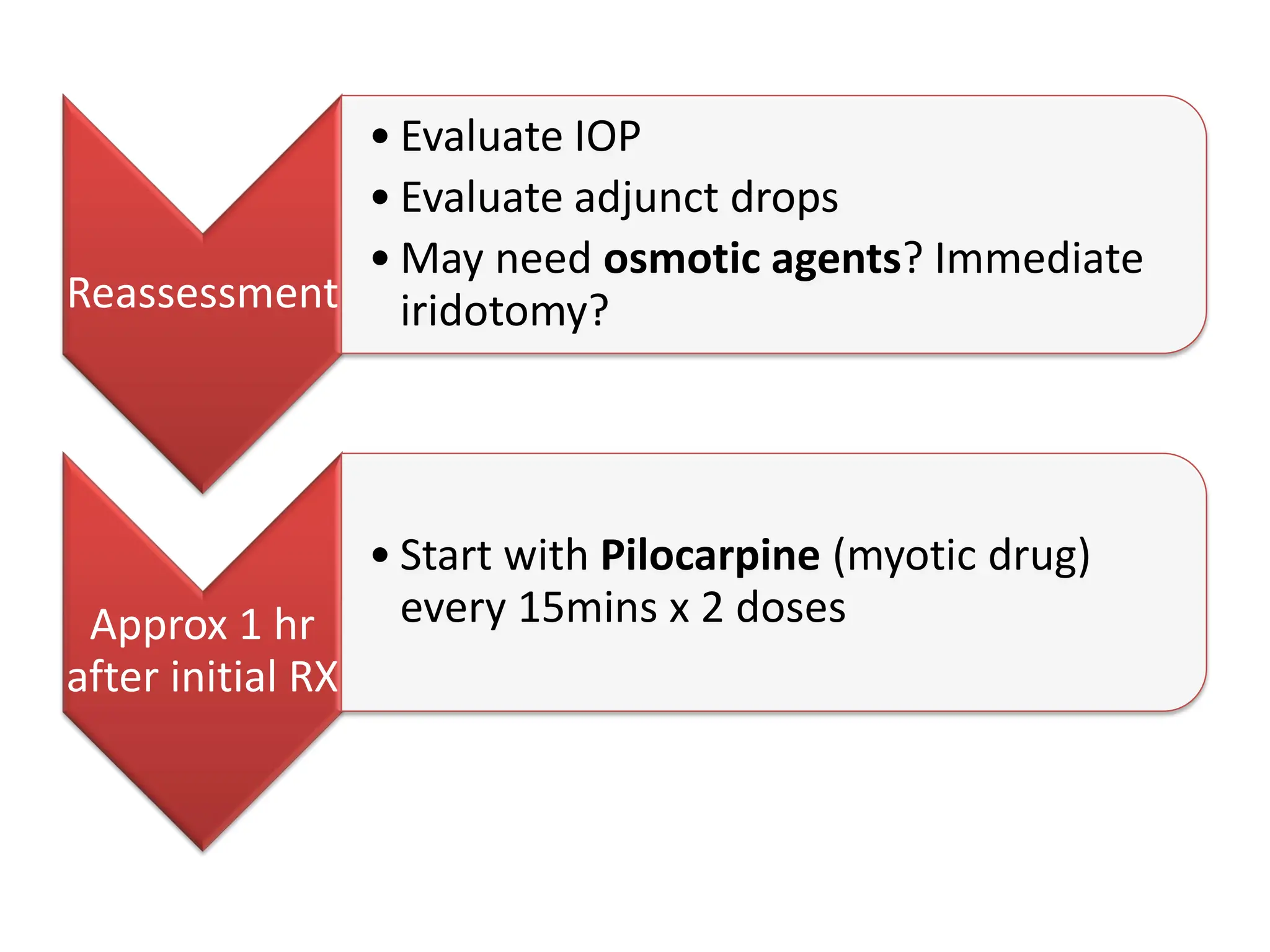
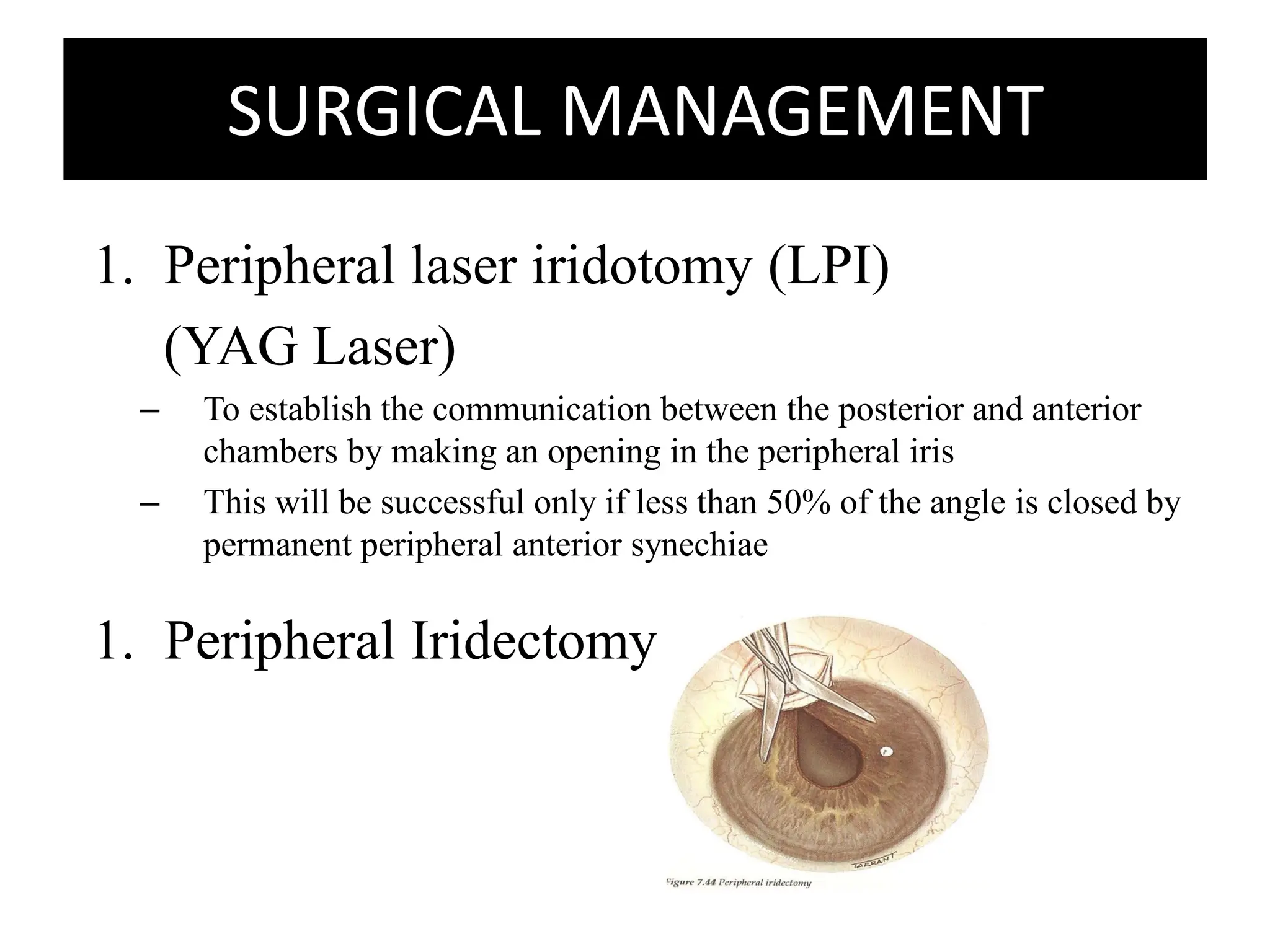
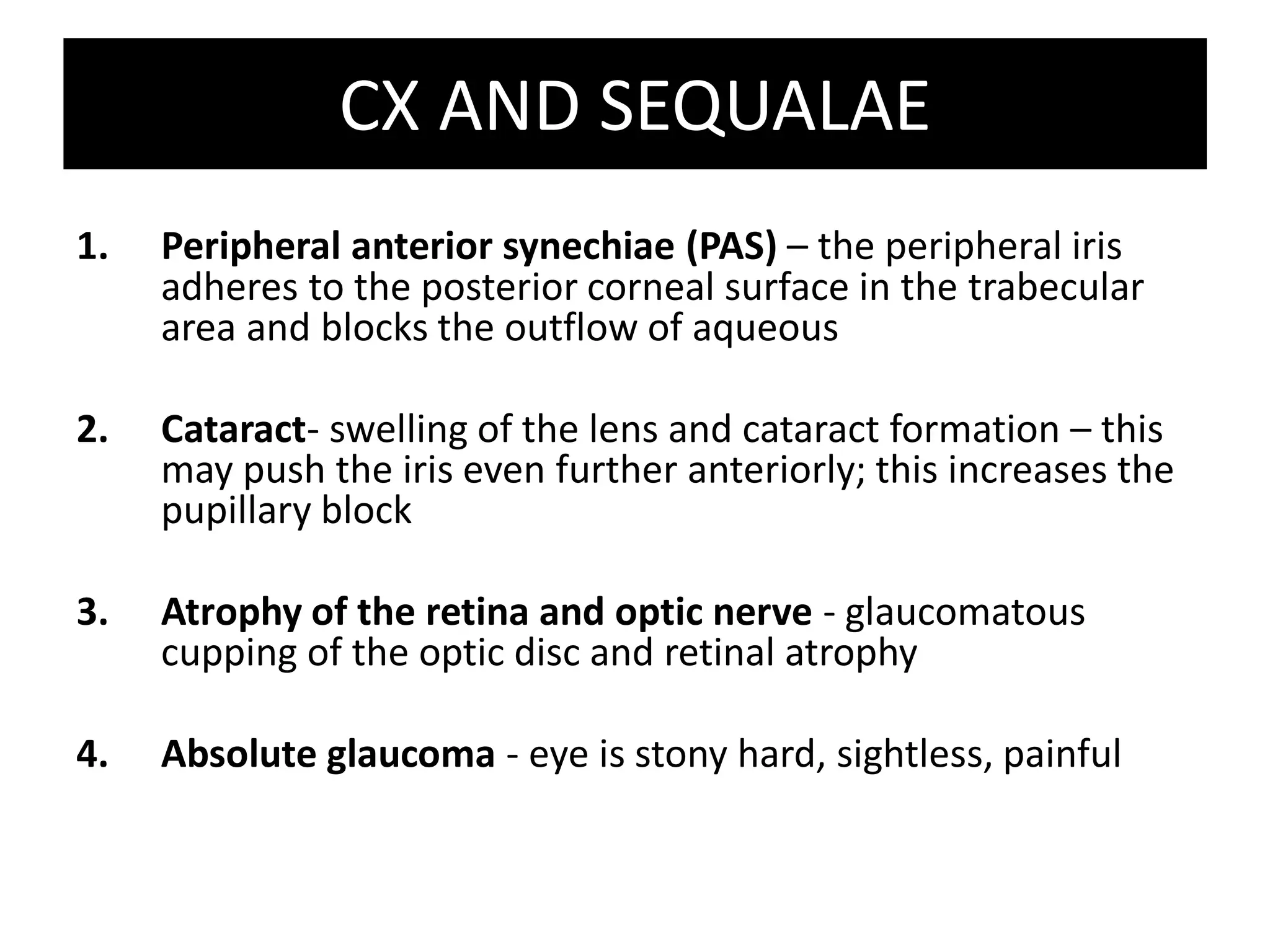
Angle-closure glaucoma is characterized by a closed anterior chamber angle that obstructs aqueous humor drainage from the eye, increasing intraocular pressure. It can be acute or chronic. Acute angle-closure glaucoma causes a rapid rise in pressure leading to pain, blurred vision, nausea, and elevated eye pressure. Treatment involves medications to lower pressure and laser or surgery to reopen the angle to restore drainage. Without treatment, permanently high pressure can damage the optic nerve and cause vision loss from glaucoma.