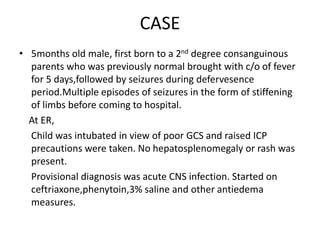
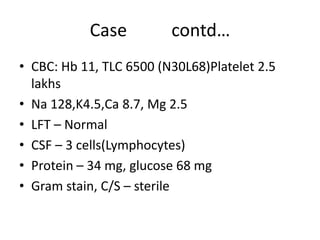
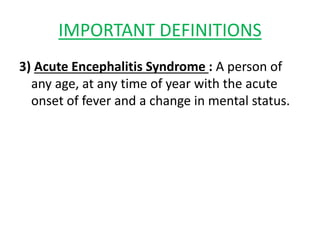
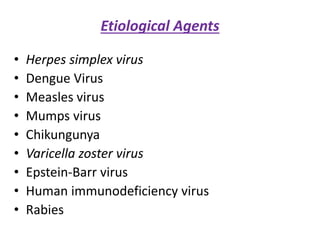
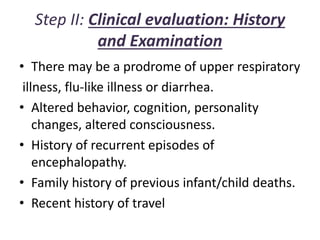
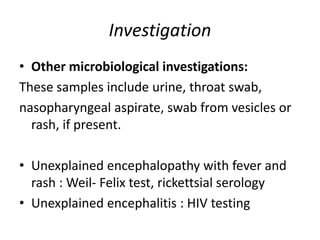
1) A 5-month-old male child presented with 5 days of fever followed by seizures and was intubated due to poor condition and raised intracranial pressure. Infectious etiologies like dengue and autoimmune encephalitis were considered.
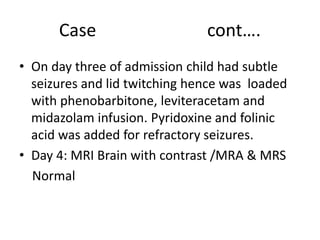
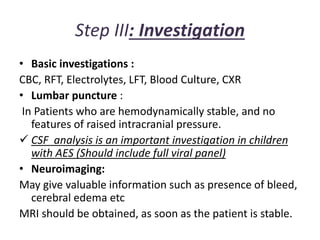
2) Investigations like MRI, LP, and metabolic workup were normal or negative. The child had refractory seizures and raised ICP and died.
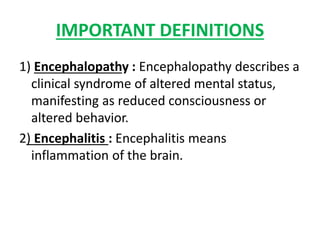
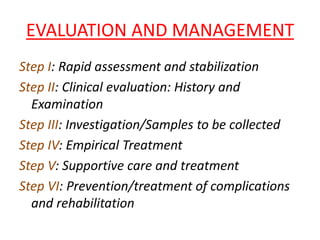
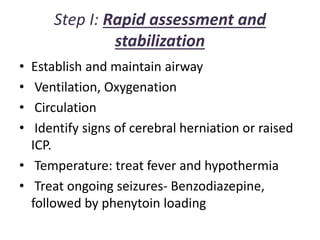
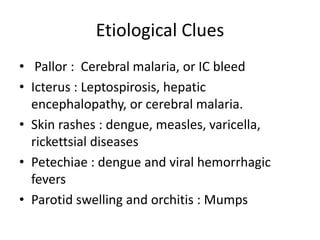
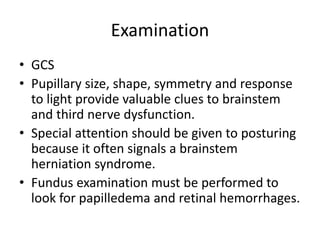
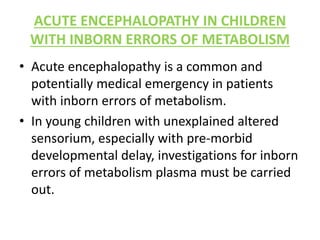
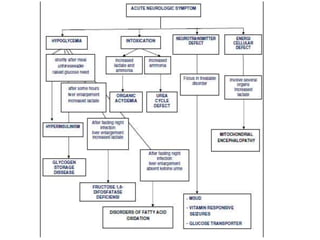
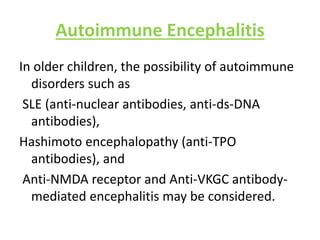
3) Causes of acute encephalopathy like infection, autoimmune, metabolic and epileptic encephalopathy were discussed. Management involves stabilization, empiric antibiotics, supportive care, preventing complications, and identifying specific causes.