This document discusses a case of neonatal diabetes mellitus (NDM) in an infant. Key points:
1. The infant presented with hyperglycemia after birth and was diagnosed with NDM after ruling out other causes.
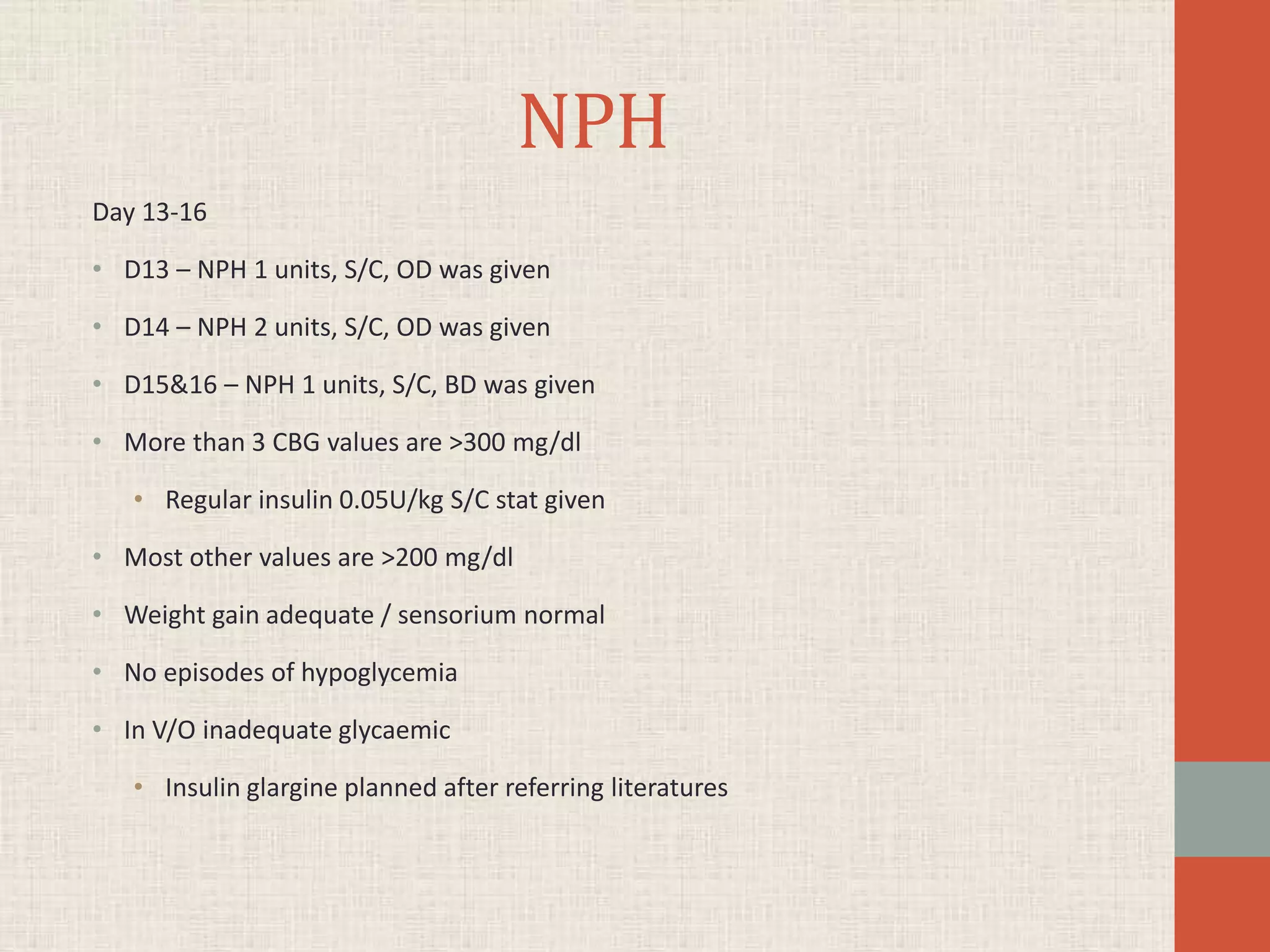
2. Treatment with NPH insulin was initially tried but glycemic control remained inadequate.
3. Insulin glargine was then started and provided excellent glycemic control with no episodes of hypoglycemia, allowing the infant to be shifted to a step-down unit.
4. NDM is a rare condition characterized by persistent hyperglycemia within the first month of life requiring insulin treatment. It can be transient or permanent and is caused by defects in insulin secretion