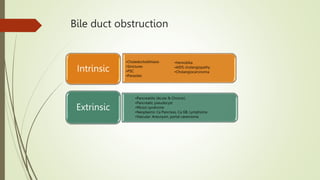
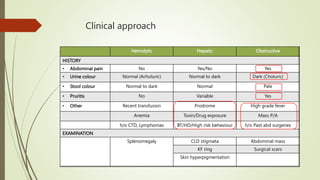
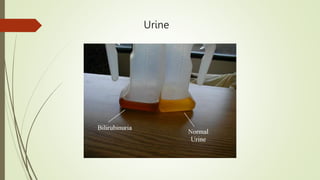
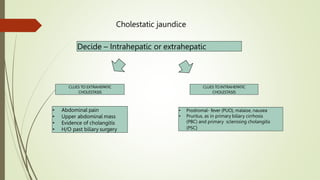
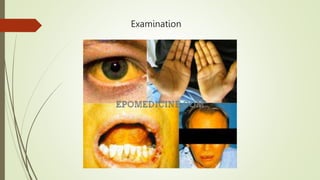
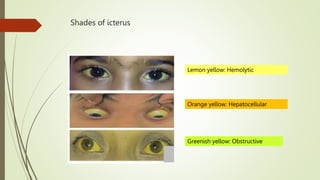
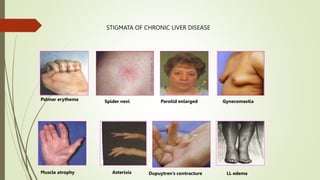
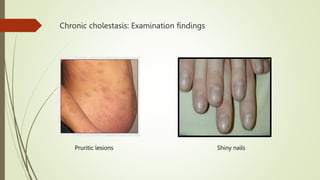
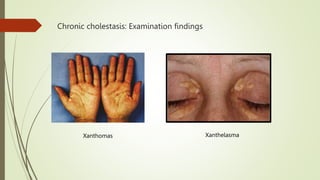
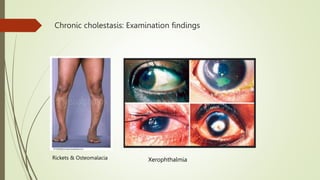
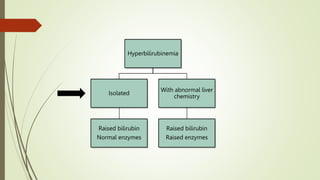
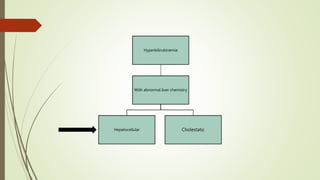
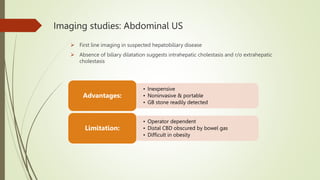
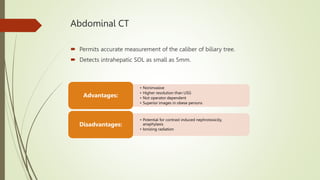
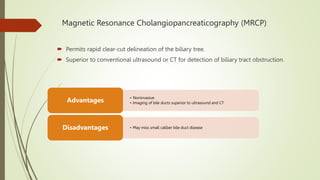
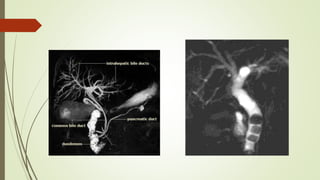
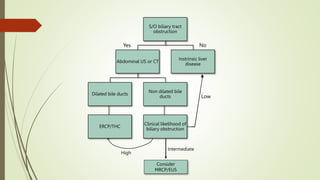
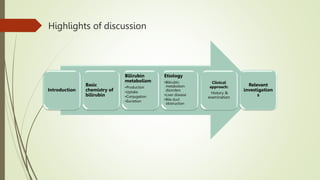
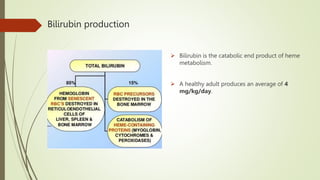
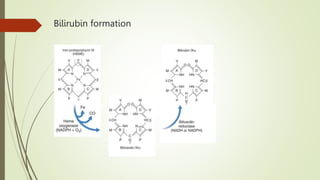
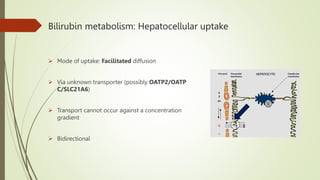
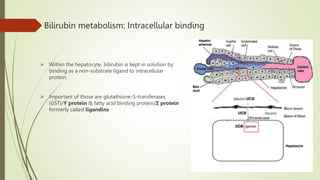
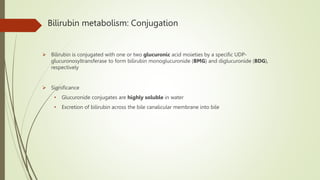
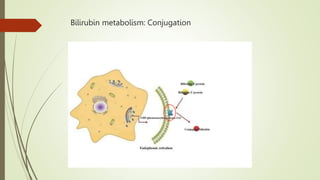
The document discusses jaundice, its history, basic bilirubin chemistry, metabolism, and clinical approach. It details the etiology of bilirubin metabolism disorders, liver diseases, and the importance of diagnostic investigations. A structured clinical approach to identify liver dysfunction and assess bilirubin pathologies is emphasized, including various imaging techniques and their advantages and limitations.



![Etiology
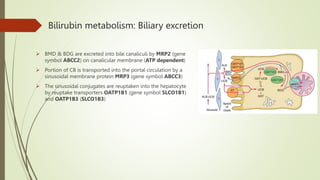
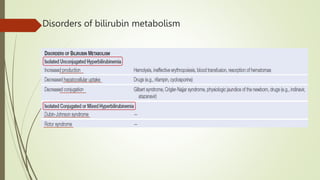
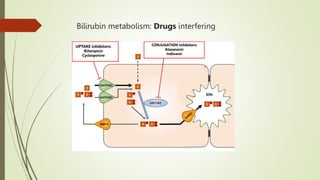
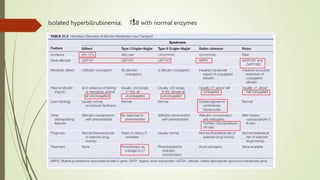
Bilirubin metabolism disorders
(Isolated hyperbilirubinemia)
• Unconjugated
Hyperbilirubinemia
• Conjugated or Mixed
Hyperbilirubinemia
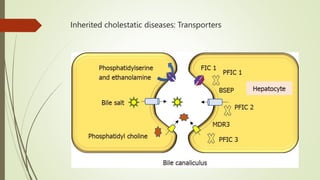
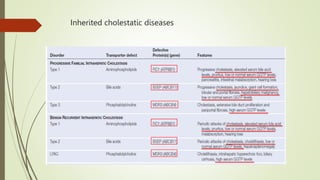
Liver Disease
• Hepatocellular
Dysfunction
• Hepatic Disorders with
Prominent Cholestasis
[INTRAHEPATIC]
Obstruction of the Bile
Ducts [EXTRAHEPATIC]
• Intrinsic causes
• Extrinsic causes](https://image.slidesharecdn.com/approachtojaundice-230605183535-595d93ae/85/Approach-to-Jaundice-16-320.jpg)
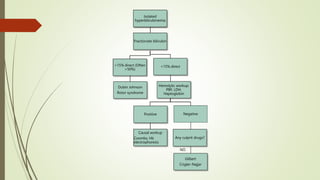
![Etiology
Bilirubin metabolism disorders
(Isolated hyperbilirubinemia)
Liver Disease
Obstruction of the Bile
Ducts [EXTRAHEPATIC]](https://image.slidesharecdn.com/approachtojaundice-230605183535-595d93ae/85/Approach-to-Jaundice-20-320.jpg)

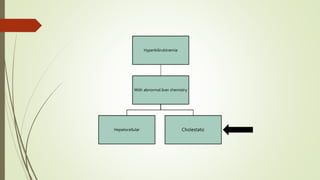
![Etiology
Bilirubin metabolism disorders
(Isolated hyperbilirubinemia)
Liver Disease
Obstruction of the Bile
Ducts [EXTRAHEPATIC]](https://image.slidesharecdn.com/approachtojaundice-230605183535-595d93ae/85/Approach-to-Jaundice-24-320.jpg)