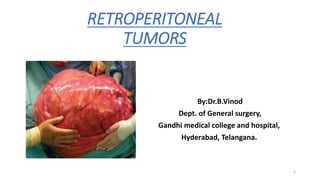
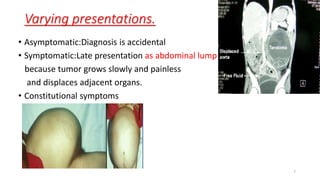
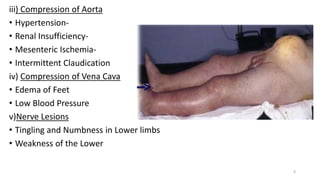
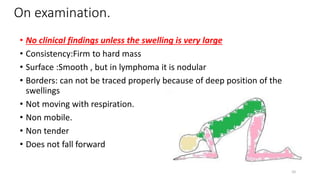
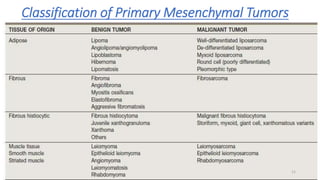
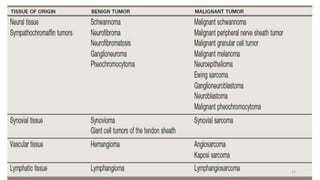
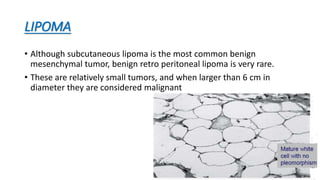
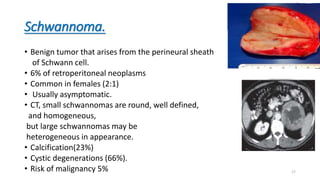
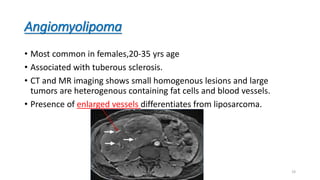
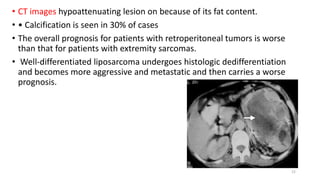
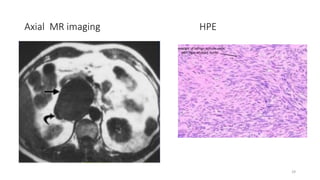
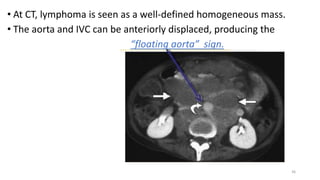
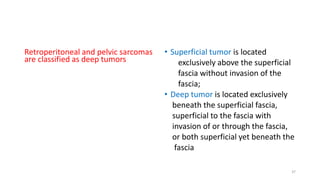
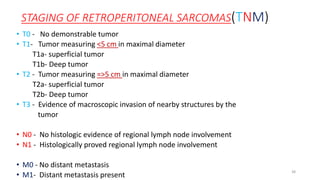
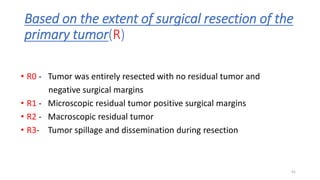
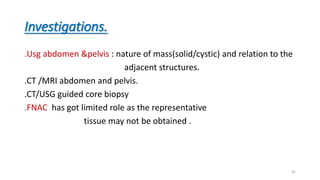
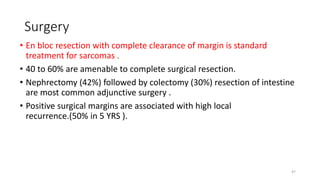
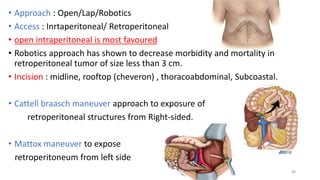
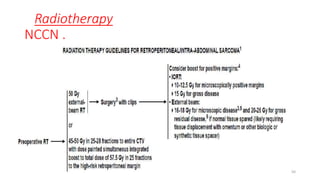
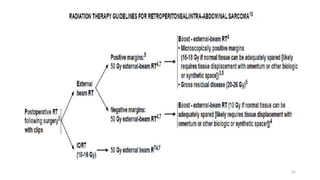
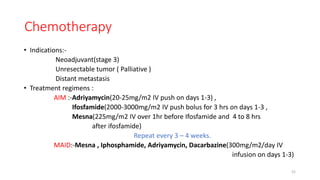
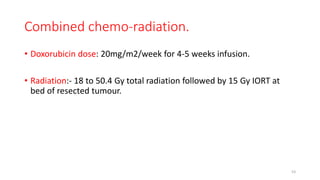
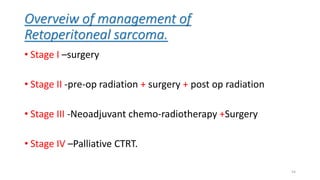
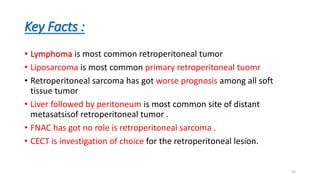
Primary retroperitoneal tumors are rare neoplasms that arise in the retroperitoneum and pelvis. Liposarcoma is the most common type of primary retroperitoneal tumor, while lymphoma is the most common retroperitoneal malignancy overall. These tumors often grow extensively before causing symptoms. Diagnostic imaging includes CT or MRI to evaluate the tumor characteristics and relationship to surrounding structures. Surgical resection with negative margins is the standard treatment for localized primary retroperitoneal sarcomas, while chemotherapy or radiation may be used in certain settings. Prognosis depends on tumor grade, stage, and ability to achieve a complete resection.