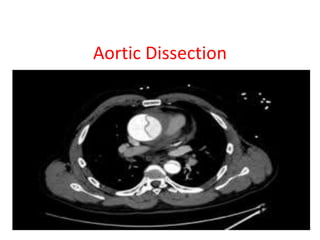
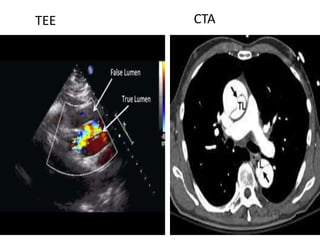
- Aortic dissection involves separation of the aortic media from the adventitia, creating a true and false lumen. It can be acute or chronic.
- Risk factors include hypertension, connective tissue disorders, congenital issues, trauma, pregnancy, and certain drugs or syndromes.
- It is classified using the Stanford or De Bakey system and usually affects those 50-70 years old, though it can occur in younger people with conditions like Marfan syndrome. Left untreated, it has a high mortality rate within weeks.